What is the biggest thing you can put into your mouth and bite into it without breaking your jaw? You may say an apple, or an orange, a cupcake, a sandwich, etc. If you had a mouth gape as large as American Isaac Johnson, the biggest food you can fit into your mouth is 10.196 cm (4.014 in) wide. That would be equivalent to a grapefruit, a small pie or tart, or a large hamburger, a large cookie, a large cinnamon roll, flatbread or Yorkshire pudding. If you tried to fit in much larger food into your mouth, it would be extremely difficult. People would tell you to 'don't bite off more than you can chew'.
Or can you?
The act of biting involves a set of teeth clamping down on an object for the purposes of eating, foraging, hunting, play, fighting, self-defence or killing.
What are teeth?

- Located in the jaws (or mouths) and covered in gums, teeth are a firm, calcified structure that organisms (e.g. carnivores and omnivores) use to disintegrate food, capture or injure prey, intimidate other animals, defend against enemies, or carry prey or their young.
- A common misconception about teeth is they are made of bone. In fact, teeth are composed of multiple tissues of varying density and sturdiness that originate from the ectoderm, the outermost embryonic germ layer.
- Douglas Harper found the word tooth originates from the Proto-Germanic *tanþs derived from the Proto-Indo-European *h₁dent-, which consisted of the root *h₁ed- ("to eat") plus the active participle suffix -nt, therefore literally meaning "that which eats".
- The irregular plural form teeth is due to Germanic umlaut whereby vowels immediately preceding a high vocalic in the following syllable were raised.
- As the nominative plural ending of the Proto-Germanic consonant roots (to which *tanþs belonged) was *-iz, the root vowel in the plural form *tanþiz (altered by this point to *tą̄þi via unrelated phonological processes) was raised to /œː/, and later unrounded to /eː/. This resulted in the tōþ/tēþ alternation attested from Old English.
- Cf. also Old English bōc/bēċ, "book/books" and mūs/mȳs, "mouse/mice", from Proto-Germanic *bōks/bōkiz and *mūs/mūsiz respectively.
Describe the origins of teeth
- It is assumed that teeth evolved from either ectoderm denticles (i.e. scales) that folded and integrated into the mouth (known as the "outside-in" theory), or endoderm pharyngeal teeth (mainly formed in the pharynx of jawless vertebrates (known as the "inside-out" theory).
- Nasoori (2020) theorised that the neural crest gene regulatory network and neural crest-derived ectomesenchyme play key roles in producing teeth.
- Sharpe (2001) found the genes determining tooth development in mammals are homoglous to those involved in the development of fish scales.
- Jennifer Viegas (2015) discovered the teeth and scales of an extinct fish species called Romundina stellina were composed of the same tissues, which is also found in mammal teeth. This supports the theory that teeth evolved as a transformation of scales.
Mammal teeth
i. Afrotherians
- Elephants / Proboscideans
- At birth, elephants have a total of 28 molar plate-like grinding tooth excluding the tusks. They are organised into 4 sets of 7 consecutively larger teeth which the elephant gradually wears through during its lifetime of chewing rough plant material.
- Only 4 teeth are involved in the chewing process at a given time. As one tooth wears out, another tooth shifts forward to replace it. The last and largest of these teeth typically becomes exposed when the proboscidean is around 40 years of age, and tend to last for an extra 20 years.
- Burton & Burton (2002) found elephants won't be able to chew food once the last of their teeth fall out regarding of its age, thus will die of starvation.
- Elephants have a pair of tusks that serve as specialised incisors for fighting, digging up food and boring tools.
ii. Carnivorans
- Meiri, Dayan & Simberloff (2005) describe carnassials as specialised teeth used by carnivores to slice through flesh. It is theorised either the molars or both the premolars and molars in combination may have modified into shearing carnassials. This suggests carnivore teeth are influenced by the animals' diets.
- Pérez-Ramos et al. (2019) discovered the space a tooth root occupied indicated the bite force required from the species. e.g. Panda teeth had the deepest root systems due to their bamboo diet.
iii. Humans
- Like most mammals, humans are diphyodont, meaning they develop 2 sets of teeth. The first set is known as deciduous teeth, also referred to as "baby teeth", "milk teeth", or "primary teeth".
Describe the development of human teeth
- Known as odontogenesis, tooth development is a complicated process by which teeth form from embryonic cells, develop and erupt into the mouth. In order to achieve a healthy oral environment, every aspect of the tooth has to develop during appropriate stages of foetal development.
- The tooth germ is an aggregation of cells that originate from the ectoderm of the first pharyngeal arch and the ectomesenchyme of the neural crest. In addition, the tooth germ is arranged into three components: the enamal organ, the dental papilla and the dental sac or follicle.
- The enamal organ consists of the outer enamel epithelium, inner enamel epithelium, stellate reticulum and stratum intermedium.
- These cells generate ameloblasts, which produce enamel to form part of the reduced enamel epithelium (REE) after maturation of the enamel. The cervical loop is where the outer enamel epithelium and inner enamel epithelium combine.
- When cervical loop cells develop into the deeper tissues, they form the Hertwig Epithelial Root Sheath, which forms the root shape of the tooth. Researchers found keratin in the epithelial cells of the tooth germ, as well as a thin layer of keratin in an erupted tooth (i.e. Nasmyth's membrane or enamel cuticle).
- The dental papilla contains cells that develop into dentin-producing cells called odontoblasts. Furthermore, the junction between the dental papilla and inner enamel epithelium dictates the crown shape of the tooth. Development of the tooth pulp is determined by the mesenchymal cells within the dental papilla.
- The dental sac or follicle produces three types of cells: cementoblasts, fibroblasts, and osteoblasts. Cementoblasts produce cementum of the tooth, while osteoblasts produce the alveolar bone around the roots of the tooth. Moreover, Rose et al. (2003) found fibroblasts give rise to the periodontal ligament that links the tooth to the alveola bone through cementum.
- Christensen et al. (1993) found NGF-R within the condensing ectomesenchymal cells of the dental papilla in the early cap stage tooth germ, which Mitsiadis et al. (1992) found plays a number of important roles during morphogenetic and cytodifferentiation events in the tooth.
- A number of studies found all stages, growth and morphogenesis of the tooth are regulated by a protein called sonic hedgehog (Sh).
Human tooth development timeline
Describe the stages of human tooth development
1. Initiation Stage
- The earliest sign of a tooth forming is the microscopic distinction between the vestibular lamina and the dental lamina. This stage occurs in the 6th - 7th week of embryonic development. The dental lamina joins the developing tooth bud to the epithelial layer of the mouth.
2. Bud stage
- During this stage, the tooth bud appears without a clear arrangement of cells. This stage technically starts once the epithelial cells proliferate into the ectomesenchyme of the jaw. The tooth bud manifests itself as a collection of cells at the periphery of the dental lamina. This usually occurs when the foetus is approximately 8 weeks old.
- Along with the development of the dental lamina, about 10 round epithelial structures (buds) form at the distal aspect of the dental lamina of each arch. These correspond to the 10 primary teeth of each dental arch.
- Each bud is separated from the ectomesenchyme by a basement membrane. Ectomesenchymal cells gather deep to the bud, creating a collection of cells, which signifies the start of condensation of the ectomesenchyme.
3. Cap stage
- The cells in the tooth bud begin their arrangement during this stage. A small collection of ectomesenchymal cells halt production of extracellular substances, which leads to an aggregation of these cells known as the dental papilla.
- The tooth bud then develops around the ectomesenchymal aggregation, looking like a cap, which becomes the enamel organ enveloping the dental papilla. An aggregation of ectomesenchymal cells called the dental sac or follicle surrounds the enamel organ and inhibits the dental papilla.
- Ultimately, the enamel organ produces enamel, the dental papilla produces dentin and pulp, and the dental sac produces all the supporting structures of a tooth such as the periodontium.
4. Bell stage
- During this stage, the dental organ is bell-shaped, and a majority of its cells are known as stellate reticulum due to its star-shaped appearance.
- Cells on the periphery of the enamel organ split into 4 different layers.
- Cuboidal cells on the periphery of the dental organ are called the outer enamel epithelium (OEE).
- The columnar cells of the enamel organ of the enamel organ next to the enamel pailla are called the inner enamel epithelium (IEE).
- The cells situated between the IEE and the stellate reticulum form a layer called the stratum intermedium.
- The rim of the enamel organ where the OEE and IEE connect is called the cervical loop.
- Meanwhile, the dental lamina disintegrates, which separates the developing teeth from the epithelium of the oral cavity. They won't connect again until the final tooth eruption into the mouth.
- The shape of the inner enamel epithelium determines the shape of the crown of the tooth. Although all teeth undergo the same process, researchers don't understand why this leads to a variety of crown shapes e.g. incisors compared to canines.
- The first hypothesis is the "field model", which suggests the existence of components for each type of tooth shape within the ectomesenchyme during tooth development. It is proposed that certain components for specific types teeth are confined to one area and scatter in different areas of the mouth.
- The 2nd hypothesis is the "clone model", which suggests the epithelium signals a group of ectomesenchymal cells to produce teeth of particular shapes. This group of cells is called a clone, which manoevres the dental lamina into tooth development, resulting in the formation of a tooth bud.
- The growth of the dental lamina continues in an area known as the "progress zone". Once the progress zone travels a fair distance from the first tooth bud, a 2nd tooth bud begins to develop.
- Note these 2 models aren't necessarily mutually exclusive, nor are widely accepted by the dental science community.
- Other areas that could form in the developing tooth during this stage include the enamel cords, enamel knots, and enamel niche.
5. Advanced bell stage
- During this maturation stage, IEE cells undergoing mitosis halt their proliferation at the location where the cusps of the teeth form, which yields the first mineralised hard tissues such as dentin and enamel. Simultaneously, IEE cells transform from cuboidal to columnar to become preameloblasts.
- The nuclei of these cells shift closer to the stratum intermedium and further from the dental papilla as they become polarised.
- The adjacent layer of cells in the dental papilla enlarges and differentiates into odontoblasts, which are the cells that produce dentin.
- This indicates changes in the IEE essentially leads to the formation of odontoblasts from the tips of the cups, thereby releases a substance, an organic matrix, into their surrounding. This organic matrix contains the components required for the production of dentin.
- As odontoblasts release organic matrix called predentin, they move toward the centre of the dental papilla. Therefore, dentin begins appearing in the surface adjacent to the outside of the tooth and proceeds inward. In addition, odontoblasts leave behind cytoplasmic extensions during its inward migration. The tubular microscopic appearance of dentin is caused by dentin forming around these extensions.
- When the production of dentin initiates, the cells of the IEE release an organic matrix against the dentin, which mineralises and becomes the first layer of the tooth's enamel. New ameloblasts form outside the dentin in response to the creation of dentin, which continue the process of enamel production.
Describe the formation of the hard tooth
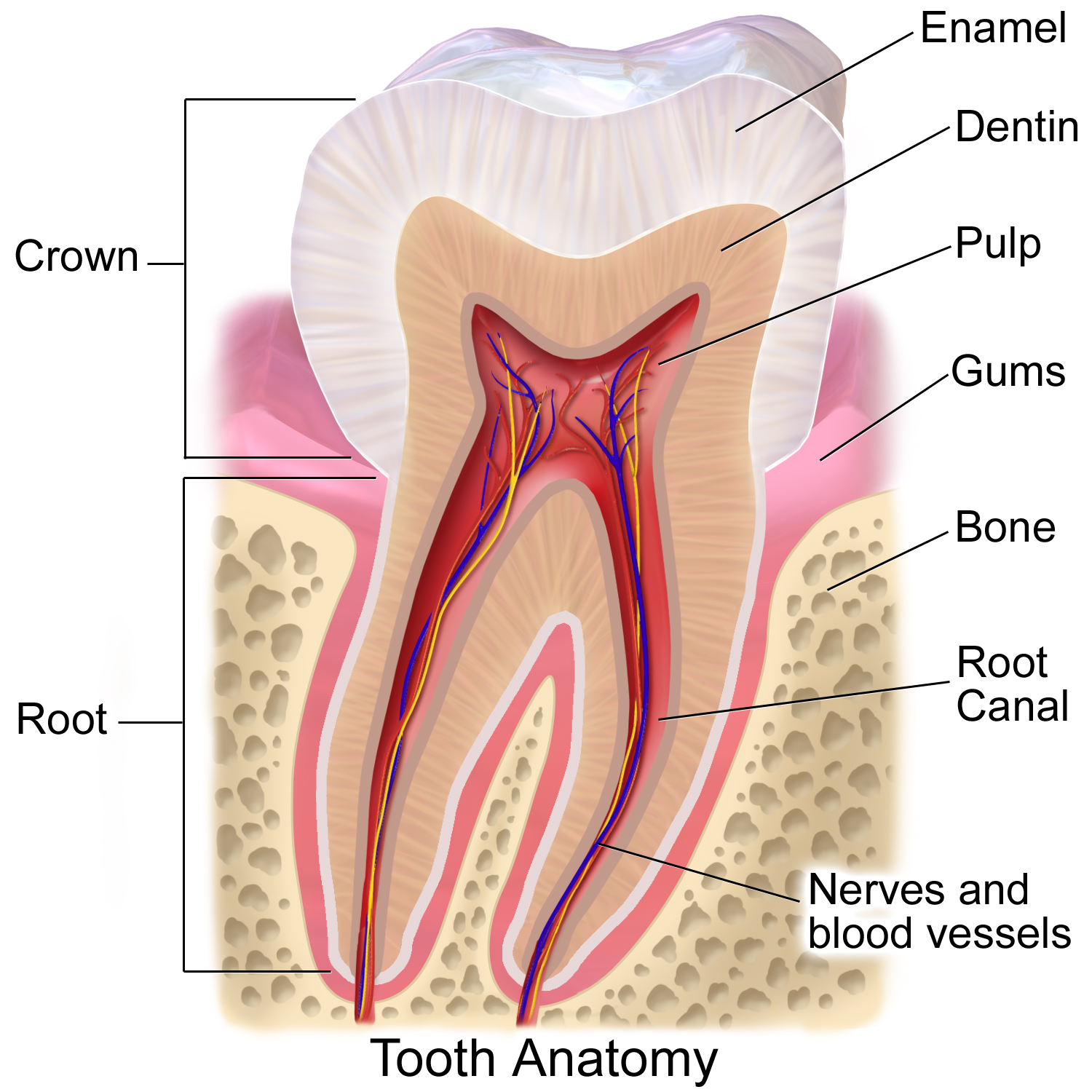
i. Enamel
Tooth enamel is an extremely hard, white to off-white, mineralised substance that shields the tooth. However, it is vulnerable to deterioration, especially after exposure to acidic food and drink.
Describe the development of enamel
- The name of the process of the formation of enamel on teeth is called amelogenesis. Enamel starts to form when the crown is appearing during the advanced bell stage of tooth development after the first layer of dentin forms as a result of dentinogenesis.
- A 2011 Elsevier article stated that 'reciprocal induction' determines the relationship between the production of dentin and enamel. It is critical that dentin must form before enamel begins to form. At this period, the dentin hasn't mineralised and there is a basal lamina situated between the IEE and the dental papilla.
- The differentiation phase begins when the predentin is newly produced. The IEE cells then lengthen and transform into preameloblasts. Each preameloblast then enlarges to become a polarised, post-mitotic, and secretory ameloblast.
- A signal is transmitted from the newly differentiated ameloblasts across the dentinoenamel junction (DEJ) to trigger dentinogenesis.
b. Secretory stage
- In this stage, ameloblasts become polarised columnar cells. They release enamel proteins into the surrounding area and help grow the enamel matrix, which is subsequently mineralised by an enzyme called alkaline phosphatase.
- When the first layer of enamel is created, the ameloblasts shift away from the interface with dentin, making provisions for the development of Tomes' processes at the end of the cell in contact with the DEJ.
- Tomes' process is defined as the end of the cell establishing the crystals of the enamel matrix. They are angled, which creates differences in crystallite orientation, and thus structure.
- Enamel continues to form around the neighbouring ameloblasts, leading to a pit that accommodates a Tomes' process. Moreover, enamel forms around the end of each Tomes' process, leading to a deposition of enamel matrix within each pit.
- The matrix within the pit eventually forms an enamel rod, and the walls eventually forms the inter-rod enamel. The only distinguishing factor between an enamel rod and an inter-rod enamel is the orientation of the calcium crystals.

c. Maturation stage
- In this stage, the ameloblasts transport molecules involved in the formation of enamel. The ameloblasts become striated, which indicates their function has changed from production to transportation.
- The proteins involved in the mineralisation process produce a majority of the material transported into the matrix include amelogenins, ameloblastins, enamelins, and tuftelins. It is still unclear how these proteins are released into the enamel structure. Cantù et al. (2017) suggested the Wnt signalling proteins BCL9 and Pygopus may be involved in amelogenesis, but their roles aren't well understood.
- The calcium ions primarily originates from the enamel organ by either active, intracellular transportation or passive, extracellular transportation. The active pathway is mediated by ameloblasts, thus the site of mineralisation is heavily regulated, including the modulation of proteins that inhibit mineralisation (e.g. serum-derived albumin) and the concentrations of ions.
- During enamel production, mineralisation occurs when calcium ions deposit between nanospheres of amelogenins forming crystallites. The newly created enamel begins to mature by thickening the long, thin prisms of hydroxyapatite, removing amelogenins and a majority of non-amelogenins from the matrix in order to provide more space for hydroxyapatite deposition.
- A 2013 Ten Cate's Oral Histology article described mature crystals as hexagonal in shape, 25 x 75 nm and runs the whole length of the enamel (~ 2.5 mm).
- During the mineralisation process, the enamel continuously becomes less porous. When amelogenins and ameloblastins are withdrawn after use, with enamelins and tuftelin remaining in the enamel, mineralisation of enamel is completed.
- After the maturation stage, but prior to the tooth erupting into the mouth, the ameloblasts apoptosise. As a consequence, enamel is unable to be regenerated by itself. This means the body nor a dentist cannot repair any damaged enamel tissue from decay or injury.
- After the mineralisation step is finished, amelogenesis process is complete.
Enamel is covered by the following structures in relation to tooth development:
-- Nasmyth membranes / enamel cuticle = Derived embryologically that is composed of keratin resulting in the enamel organ.
-- Acquired pellicle = Derived after tooth eruption that is composed of food debris, calculus, dental plaque (organic film).
Progress of enamel formation for primary teeth
Describe the features of enamel
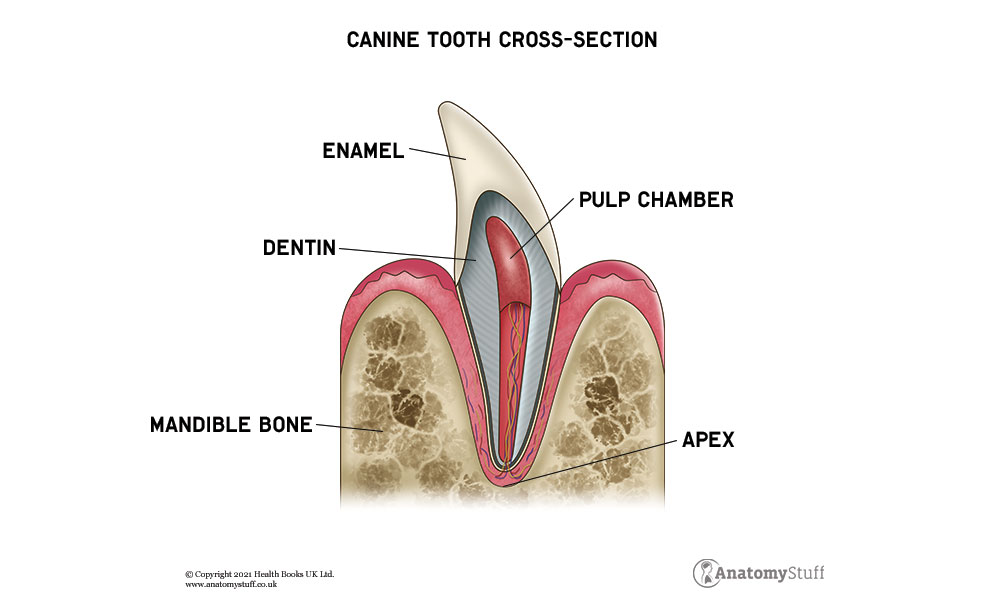
- Enamel is arguably the hardest material in the human body, containing the highest proportion of minerals (~ 96%), with the remaining consisting of water and organic material. Staines et al. (1981) identified the primary mineral of enamel is a crystalline calcium phosphate called hydroxyapatite.
- Enamel is usually thickest at the cusp (~ 2.5 mm), and thinnest at the border with the cementum at the cementoenamel junction (CEJ).
- The colour of enamel varies from light yellow to greyish white, which may be determined by differences in the translucency of enamel. Yellowish teeth tend to have a thin, translucent enamel, which allows the yellow dentin to be visible and greyish teeth tend to have a more opaque enamel.
- Variations in translucency of the enamel may be determined by the level of calcification and the homogeneity of the enamel. There is no dentin underneath the enamel at the edges of the tooth, which makes the tooth appear blue-ish or translucent off-white.
- Since enamel is semitranslucent, the colour of dentin and any substance beneath the enamel influences the appearance of a tooth. The enamel on primary teeth has a relatively opaque crystalline form and thus looks whiter than on permanent teeth.
- The more enamel a tooth contains, the stronger it becomes, however it becomes more brittle. Tooth enamel is ranked 5 on the Mohs hardness scale (harder than steel and softer than titanium) and has a Young's modulus of 83 GPa. On radiographs, enamel's appear lighter than dentin or pulp because it is denser and more opaque than both dentin and pulp.
- Enamel contains two classes of proteins called amelogenins and enamelins, which are thought to serve as a framework for minerals to develop on as part of enamel development.
- Enamel doesn't contain any collagen, soft organic matter, blood vessels and nerve supply, however it isn't a static tissue due to its ability to undergo mineralisation changes.
Describe the structure of enamel
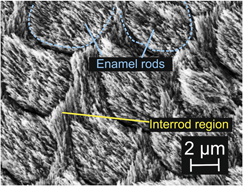
- The basic unit of enamel is an enamel rod, which is 4–8 μm in diameter. It is a compact mass of hydroxyapatite crystallites in an organised pattern. A cross section of an enamel rod shows the top (or head) oriented toward the crown of the tooth, and the bottom (or tail) oriented toward the root of the tooth.
- In the head of the enamel rod, enamel crystallites are oriented parallel to the long axis of the rod. In comparison, enamel crystallies in the tail of the enamel rod are oriented about 65 degrees from the long axis.
- Enamel rods are arranged in rows along the tooth, and within each row, the long axis of the enamel rod is perpendiular to the underlying dentin. In permanent teeth, the enamel rods located adjacent to the cementoenamel junction (CEJ) lean slightly toward the root of the tooth.
- The region around the enamel rod is called the inter-rod enamel, which shares the same composition but has a crystallite orientation as the enamel rod. The border where the enamel rods and the interrod enamel converge is called the rod sheath.
- The brown-ish incremental lines in mature enamel are called striae of Retzius, which are composed of bands or cross striations on the enamel rods that traverse them when integrated in longitudinal sections. Created from changes in the diameter of Tomes' processes, these incremental lines indicate enamel growth.
- There is debate on the exact process that forms these incremental lines. Some researchers theorise the lines are a product of the circadian, metabolic rhythm of the ameloblasts producing the enamel matrix, which comprises of an active secretory work period succeeded by an inactive rest period. Therefore, each band on the enamel rod indicates the work / rest pattern of the ameloblasts that occur over a week.
- The shallow grooves on the non-masticatory surfaces of a number of teeth in the oral cavity are referred to as perikymata. Bath-Balogh & Fehrenbach found perikymata erodes through tooth wear, except on the protected cervial areas of certain teeth, particularly the canines, first premolars and the maxillary central incisors.
- The neonatal is an incremental line that splits the enamel formed before and after birth, which indicates the stress experienced by the ameloblasts during birth. It appears darker than other incremental lines, which is associated with the sensitivity of the ameloblasts during the formation of enamel matrix.
- The neonatal line is situated in all primary teeth and in the larger cusps of the permanent first molars.They comprise irregular structures of enamel prisms with disordered crystallite arrangements formed by the sharp curvature of the prisms towards the root.
- Gnarled enamel is situated on the cusps of teeth that appears twisted because of the orientation of enamel rods and the rows in which they sit in.
What factors lead to loss of enamel loss?
- Since enamel has a higher mineral content, it makes this tissue the hardest in the body. However, it is susceptible to demineralisation that results in dental caries, known as cavities.
- When the enamel is exposed to sugars and acids from candies, fruit juices, soft drinks or other sweet and acidic foods, it leads to dissolution of tooth enamel, which results in enamel destruction.
- When sucrose covers the surface of the mouth, a number of intraoral bacteria interact with the sucrose and produce lactic acid, which increases the acidity (or reduces the pH) in the mouth.
- When the pH reduces below 5.5, the hydroxyapatite crystallites of enamel start to demineralise, which increases the risk of bacteria entering deep into the tooth. The most common bacterium associated with tooth decay is Streptococcus mutans, but the amount and species of bacteria varies with the development of tooth destruction.
- If enamel continues to demineralise to a point when it is impossible to avoid the invasion of bacteria, the underlying dentin becomes damaged too. If dentin is eroded by a physiologic condition or by decay, the enamel won't be able to compensate for its brittle nature and breaks off from the tooth easily.
- There is a misconception that the amount of sugar consumed is associated with tooth decay. In fact, the British Nutrition Foundation stated that the frequency of sugar consumption is a major factor in tooth decay, as well as the length of time sugar remains in the mouth.
- Consumption of sugar initially reduces the pH in the mouth, which demineralises enamel and makes it susceptible for about 30 mins. Note that eating a higher amount of sugar in one sitting doesn't increase the rate of demineralisation. Likewise, consuming a reduced amount of sugar doesn't reduce the rate of demineralisation.
- Therefore, eating a high amount of sugar in one sitting in the day is less detrimental to your teeth enamel than eating a small amount of sugar in several sittings throughout the day. For instance, oral health experts recommend to eat a single dessert at dinner time rather than to consume a bag of candy throughout the day.
 |
| The effects of bruxism on an anterior tooth, revealing the dentin and pulp which are usually hidden by enamel. |
- Enamel is also vulnerable to other factors such as bruxism, abrasion (involving foreign objects, such as toothbrushes), and erosion (by chemical processes, such as dissolving by soft drinks or acidic fruit juices).
- It is a misconception that enamel erodes primarily from chewing, but actually teeth barely make contact during the act of chewing. In addition, teeth contact is usually compensated by the periodontal ligaments and the arrangement of dental occlusion.
- Xu et al. (1998) estimated tooth enamel can resist up to 1,000 N of force several times a day during the process of chewing in spite of its brittle nature being similar to glass.
- Chai et al. (2009) explained the enamel tufts within the microstructure of enamel helps stabilise fractures at the dentinoenamel junction, whereby increasing its resistance to biting force. Furthermore, the structure of the tooth also helps to decrease the tensile stresses responsible for fractures during the biting process.
Enamel in other animals
- Frandson and Spurgeon found the development of tooth enamel in animals is virtually identical to that in humans. In addition, they discovered the animals' enamel organ, including ameloblasts, and the dental papilla have similar functions to the human's enamel organ.
- Pinney found dogs are less likely to experience tooth decay than humans because their saliva has a high pH. This inhibits the formation of an acidic environment and the subsequent demineralisation of enamel. If tooth decay occurs in dogs, they can receive dental fillings just as humans do.
- The tooth enamel of dogs is susceptible to tetracycline staining, which can be treated with tetracycline antibiotic therapy at a young age.
- Martin & Randall-Bowman found the enamel and dentin layers in horse teeth are entwined with each other, which strengthens the enamel structure and elevate the enamel's wear resistance.
- Mondéjar-Fernández et al. (2021) discovered enamel or enameloid in the dermal denticles of sharks and numerous early vertebrates, which indicates it emerged before the evolution of gnathostome teeth.
- Zylberberg et al. (2015) suggested the ganoin that covers the scales of actinopterygians is derived from enamel. Bentov et al. (2012) found enamel-like substances also coat the jaws of a number of crustacea, but this is not comparable with vertebrate enamel.
Describe the mechanical properties of enamel
- White (2001) demonstrated the the fracture toughness of enamel is about 3 times greater than that of geological hydroxyapatite. The microstructure of enamel contains rod and interrod regions, which results in variation of the mechanical properties of enamel depending on the location within the microstructure. Since the mechanical properties in both rod and interrod differ, it leads to anisotropy in enamel.
- Compared to the rods, the interrods has approximately 53% and 74% decreased hardness and elastic modulus. Ge (2005) thought this leads to a composite-like hierarchical structure of enamel.
- Habelitz (2001) found the hardness and rigidity parallel to the rod axis leads to increased hardness and modulus, with modulus values between 85 and 90 GPa and hardness values between 3.4 and 3.9 GPa.
- The hardness value and elastic modulus value in the direction perpendicular to the direction of the rods are 3.0 - 3.5 GPa and 70 - 77 GPa respectively. The anisotropy between the 2 direction is estimated to be as high as 30% due partially to the structure of the material and the directionality of the rods in the c-direction. Furthermore, anisotropy is a result of the composite structure of enamel.
- Single crystallite hydroxyapatite has a relatively high hardness and Young's modulus, which may be a result of the defects in enamel, such as the existence of substitutional ions and organic materials.
- Park (2008) found the elastic modulus increases as the distance from the dentin-enamel junction (DEJ) increases within enamel. Xu (1998) found cracks in the enamel don't easily permeate the dentin, which increases the fracture toughness of the enamel.
ii. Dentin
- Dentin (or dentine) is a calcified tissue that makes up one of the four major components of teeth. It is typically enveloped by enamel on the crown and by cementum on the root, surrounding the whole pulp.
- By volume, the composition of dentin is about 45% hydroxyapatite, 33% organic material, and 22% water.
- Since it is typically appears yellow, it profoundly influences the overall colour of a tooth due to the enamel's translucency.
- Since it is less brittle and less mineralised than enamel, it plays an important role in the support of enamel. Marshall et al. (1997) rated dentin as a 3 on the Mohs scale of mineral hardness.
Describe the process of dentinogenesis
The process of dentinogenesis is performed by odontoblasts, which are biological cells situated on the outer wall of dental pulps. They differentiate from cells of the dental papilla during the late bell stage of tooth development. It expresses signalling molecules and growth factors of the inner enamel epithelium (IEE).
Development of dentin
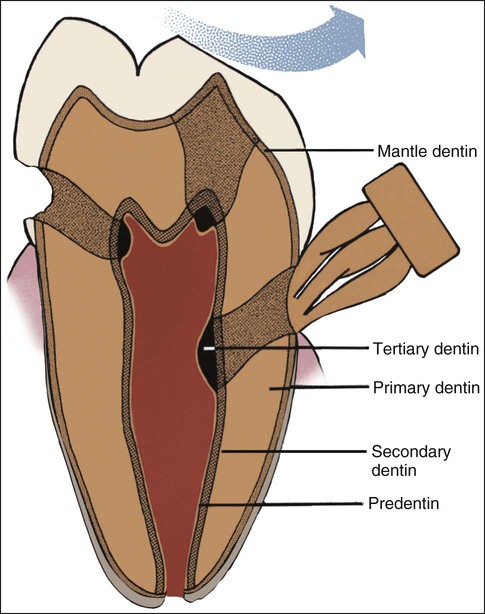
i. Mantle dentin
- Odontoblasts produce an organic matrix consisting of collagen fibres around a region directly next to the IEE, adjacent to the region of the future cusp of a tooth.
- The odontoblasts start to move toward the centre of the tooth, creating an extension called the odontoblast process. Therefore, the formation of dentin continues toward the inside of the tooth. The odontoblast process triggers the release of hydroxyapatite crystals and mineralisation of the matrix. This region of mineralisation is called the mantle dentin and is typically about 20 - 150 μm thick.
ii. Primary dentin
- Odontoblasts expand, wiping out any extracellular resources to contribute to an organic matrix for mineralisation. Furthermore, the larger odontoblasts secrete collagen in small quantities, which lead to a more tightly assembled, heterogeneous nucleation for the purpose of mineralisation.
- Located adjacent to the cervical loop of the enamel organ is the Hertwig epithelial root sheath (HERS), which is a requirement for the formation of dentin in the root of the tooth. The differences between root dentin and coronal dentin are the differing orientation of collagen fibres, phosphophoryn levels and mineralisation levels.
- Maturation of dentin or mineralisation of predentin occurs after its apposition, which transpires in 2 phases: primary and secondary.
- Firstly, the calcium hydroxyapatite crystals emerge as globules (calcospherules) in the collagen fibres of the predentin, which facilitates both the expansion and fusion of the crystals during the primary mineralisation phase.
- New sites of mineralisation start to appear as globules emerge in the partially mineralised predentin during the secondary mineralisation phase. These new sites of crystal formation are more or less uniformly layered on the earliest crystals, which allows them to enlarge and fuse.
- Globular dentin appear as lighter rounded areas on a stained section of dentin on sites where both primary and secondary mineralisation have occurred with complete crystalline fusion.
- In contrast, interglobular dentin appear as dark arc-like areas in a stained section of dentin. In these sites, only primary mineralisation has occurred within the predentin, and the globules of dentin don't fuse completely. Therefore, interglobular dentin is less mineralised than globular dentin.
iii. Secondary dentin
Secondary dentin is produced after the root of the tooth is fully formed. Note it doesn't form at a uniform rate along the tooth, but rather form quicker along areas closer to the crown of the tooth. This process continues throughout life and constitutes the smaller areas of pulp found in older individuals.
iv. Tertiary dentin
- Tertiary dentin is produced at certain sites in response to injury by odontoblasts or replacement odontoblasts from the pulp depending on the severity of the injury. Tertiary dentin can be categorised into reactionary or reparative dentin.
- Reactionary dentin is produced by odontoblasts when the injury doesn't damage the odontoblast layer, whereas reparative dentin is produced by replacement odontoblasts when the injury is sufficiently severe that it damages a section of the primary odontoblast layer.
- Therefore, a type of tertiary dentin is produced in response to stimuli, such as attrition or dental caries.
Describe the structure of dentin
- Dentin is composed of microscopic channels, known as dentinal tubules, which spread outward through the dentin from the pulp to the exterior cementum or enamel border.
- The dentinal tubules run from the dentinoenamel junction (DEJ) in the crown area, or dentinocemental junction (DCJ) in the root area, to the outer wall of the pulp. The tubules follow an sigmoidal path from the outer surface of the dentin to the region closest to the pulp.
- Dentin attenuates from the inner to the outermost surface, with a diameter of 2.5 μm near the pulp, .2 μm in the middle of the dentin, and 0.9 μm at the dentino-enamel junction.
- Its density is between 59,000 and 76,000 per square mm near the pulp, whereas its density is about half as much near the enamel.
- There is an odontoblast process within the tubules, as well as dentinal fluid, which contains albumin, proteoglycans, tenascin and transferrin. Furthermore, there are bifurcating canalicular systems that link to each other. Each are classified by size, with major branches having a diameter of 500 - 1000 nm, fine branches having a diameter of 300 - 700 nm, and micro branches having a diameter less than 300 nm.
- The major branches are located at the terminal ends of the tubules. Fine branches diverge from the dentinal tubules at 45 degree angles around every 1-2 μm, whereas microtubules diverge at 90 degree angles.
- The dentinal tubules contain the cytoplasmic extensions of odontoblasts that once produced the dentin. Marshall (1993) found the cell bodies of the odontoblasts are aligned along the inner side of dentin against a layer of predentin where they also create the peripheral boundary of the dental pulp.
- The existence of dentinal tubules adds a degree of permability to dentin, which can elevate the nociception and the rate of tooth decay. Addy (2002) hypothesised that dentinal hypersensitivity is a result of changes in the dentinal fluid associated with the processes.
- Dentin is a porous bone-like matrix that comprises of yellow-hued material. By weight, it is composed of around 70% inorganic materials (primarily hydroxylapatite and a number of non-crystalline amorphous calcium phosphate), 20% organic materials (90% of which is collagen type 1 and 10% ground substance, which includes dentin-specific proteins), and around 10% water (adsorbed on the surface of the minerals or between the crystals.
- Since dentin is softer than enamel, its rate of decay is faster than enamel and is susceptible to severe cavities if not properly treated. Due to its elastic properties, dentin provides support for enamel by preventing brittle fractures from occurring in enamel.
- In regions where both primary and secondary mineralisation have occurred with complete crystallite fusion, globular dentin appear as light rounded areas on a stained section of dentin.
- In contrast, the darker arc-like regions in a stained section of dentin are labelled interglobular dentin. These regions indicate only primary mineralisation has occurred within the predentin, and the globules of dentin haven't completely fused. Therefore, as a result, interglobular dentin is less mineralised than globular dentin.
- Interglobular dentin is observable in coronal dentin, close to the dentinoenamel junction (DEJ), and in some dental anomalies, such as dentinogenesis imperfecta.
Describe the regional variations in dentin structure and composition
- Known as the mantle dentin layer, the outermost layer is found in the crown of the tooth. Its characteristics include collagen fibres situated perpendicular to the enamel-dentin junction, and level of mineralisation being less than enamel.
- The dentin begins to mineralise when there are matrix vesicles present, which are secreted by odontoblasts, osteoblasts, and some chondrocytes. It is thought these matrix vesicles function as nucleation centres for the mineralisation process in bone, dentin, and calcified cartilage.
- There are 2 morphologically distinguishable outer layers in the root of the tooth: the hyaline layer on the periphery of dentin and the granular layer of Tomes. The granular layer appears dark and granulated due to dentinal tubules branching and looping back in this area. In contrast, the hyaline layer is clear and up to 20μm wide.
- The innermost layer of dentin is called predentin, which is in the first dentin matrix established prior to mineralisation. Predentin appears pale when stained with haematoxylin and eosin. Its width is between 10 and 40μm, depending on its rate of deposition.
Describe the microstructure of dentin
- During the dentinogenesis process, the odontoblast cells withdraw from the DEJ to the outer lining of the pulp, discarding microtubules filled with cytoplasmic extensions and leaving behind intertubular dentin (ITD) in its place.
- ITD contains a major part of the dentin and is a matrix composite of hydroxyapatite nanoparticles bundled around collagen fibres.
- Forien et al. (2015) found the mineralised collagen fibres are arrangeed in layers oriented perpendicular to the direction of the dentin microtubules. Gotliv & Veis (2007) discovered these collagen fibres are lined with peritubular dentin (PTD), which is a layer of hydroxyapatite tablets that is 1-2 μm thick with no preferred orientation and lacks any supporting collagen fibres.
- The hydroxyapatite tables within the ITD are compressed along the crystallographic c-axis due to the compact interaction between the tables and the collagen fibre.
Describe the process of crack propagation in dentin
- Tablets aligned parallel with the collagen fibres experience a considerable increase in compressive stress of around 90 MPa. In order for cracks to form, tensile stresses have to initially overwhelm the residual compressive stress.
- Since normal mastication stresses don't go beyond 40 MPa, the ITD stops the formation of cracks during normal daily use and aids in deflecting cracks perpendicular to the dentin tubule and away from the pulp.
- Crack propagation within dentin tends to travel along the interfaces of the layers of ITD. Since the hydroxyapatite tables are not preferentially orientated, they experience a smaller level of compressive residual stress, which results in microtubules serving as sites where cracks initiate.
- This leads to the formation of cross-hatched shear microcracks at the microtubules in compression and and ring-shaped microcracks in tension. The tip of a larger crack forms a stress centre that initiates microcracks around the microtubules ahead of it, which consume energy and withstand additional damage.
- Eltit et al. (2018) found microcracks imperfectly connect to a larger crack, which manifest in 'uncracked ligaments', thus halt the larger crack. In contrast, Imbeni et al. (2005) found enamel lacks the fracture resistance, and fractures running across the DEJ tend to halt within ~10 μm.
- Forien et la. (2015) discovered that the combination of the residual stress and the perpendicular orientation of the ITD mineralised collagen fibres significantly increases the fracture resistance and fatigue tolerance limit along the microtubule direction.
What are the different types of dentin?
i. Primary dentin
- The most prominent type of dentin is primary dentin, which is located between the enamel and the pulp chamber. The outer layer in close proximity to the enamel is called the mantle dentin, which is formed by newly differentiated odontoblasts and consists of a layer 15-20 μm wide.
- Compared to primary dentin, mantle dentin doesn't have phosphorylation, has less mineralisation, but contains loosely packed collagen fibrils.
- Under the mantle dentin is the circumpulpal dentin, which is more mineralised and comprises a greater proportion of the dentin layer and is produced after the mantle dentin by the odontoblasts.
- Dentin that is newly produced and hasn't undergone mineralisation is called predentin, which is about 10-47μm thick and usually lines the innermost section of the dentin. It comprises of collagen, glycoproteins, and proteoglycans.
ii. Secondary dentin
- Sometimes referred to as adventitious dentin, secondary dentin is produced after the root of the tooth is completely formed. Although the growth rate of secondary dentin is slower than that of primary dentin, it shares a similar structure to primary dentin.
- There is a greater amount of secondary dentin on the roof and floor of the coronal pulp chamber, where it shields the pulp from exposure to the environment in older teeth. As more secondary dentin is produced, the size of the pulp chamber reduces with age. This phenomenon is clinically referred to as 'pulp recession', which increases the risk of exposing the pulp during cavity preparation.
- If this occurs, a number of therapies can treat the pulp such as direct pulp capping, and adhesive dentistry.
iii. Tertiary dentin
- This type of dentin includes reparative dentin and reactionary dentin. Tertiary dentin is a product of a reaction to external stimulation such as cavities and wear.
- Reactionary tertiary dentin is formed from a pre-existing odontoblast, whereas reparative tertiary dentin is formed from newly differentiated odontoblast-like cells due to the apoptosis of the original odontoblasts.
- Since it is merely produced by an odontoblast directly influenced by a stimulus, the architecture and structure of tertiary dentin depend on the intensity and duration of the stimulus.
- For instance, if the stimulus is a carious lesion, it results in substantial scarring of dentin and damage to the pulp, due to the differentiation of bacterial metabolites and toxins. Therefore, tertiary dentin is set down swiftly to create a sparse and irregular tubular pattern and a number of cellular inclusions, resulting in "osteodentin". Osteodentin is observed in patients with vitamin A deficiency during development.
- Kinney et al. (2005) stated a stimulus that is less active reduces the rate of dentin being deposited, which results in a more regular tubular pattern and rarely any cellular inclusions.
iii. Cementum
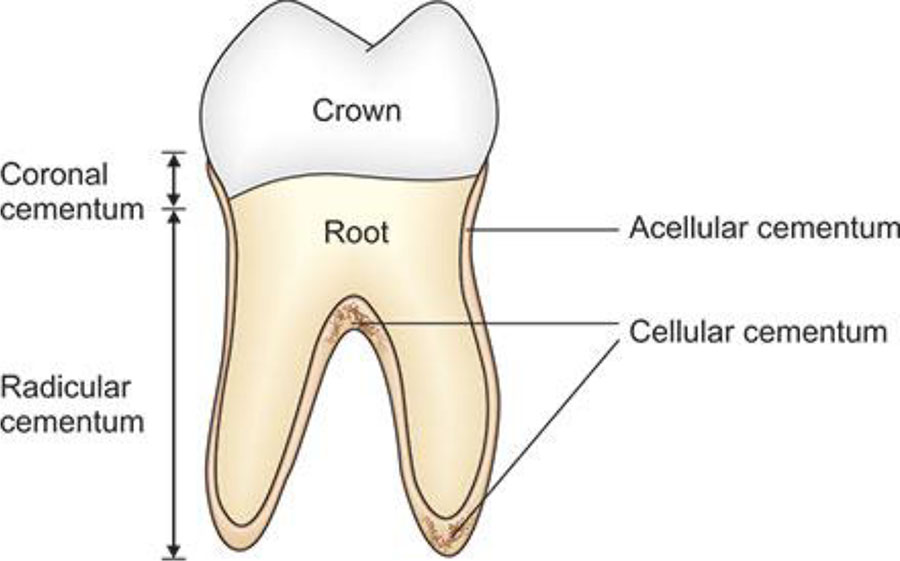
Cementum is a specialised calcified material that envelops the root of the tooth. It is part of the periodontium that connects the teeth to the alveolar bone by anchoring the periodontal ligament.
Describe the development of cementum
- Cementogenesis is initiated by the fragmentation of Hertwig epithelial root sheath (HERS). HERS is a ring of epithelial cells derived from the apical elongation of the enamel organ.
- Once the root sheath disintegrates, the newly produced surface of root dentin interacts with the undifferentiated cells of the dental follicle.
- This subsequently triggers the activation of cementoblasts to initiate cementogenesis. The external shape of each root is governed by the position of the surrounding Hertwig epithelial root sheath.
- Luan et al. (2006) theorised three possible phenomena: interruption of HERS; dentin sends a reciprocal inductive signal to infiltrating dental sac cells; transformation of HERS cells into cementoblasts.
- The cementoblasts subsequently dissipate to cover the root dentin and undergo cementogenesis, which places cementoid.
- During the latter stages within the process of apposition, a large proportion of the cementoblasts become snared by the cementum they produce, therefore becoming cementocytes.
- When the cementoid achieves adequate thickness level, it begins to mineralise around the cementocytes, subsequently becoming cementum.
- Since apposition of cementum occurs over the dentin, this results in the formation of the dentinocemental junction (DCJ).
- After the apposition of layers of cementum, the cementoblasts that aren't entrapped in cementum align along the cemental surface along the length of the outer layer of the periodontal ligament.
- These cementoblasts produce subsequent layers of cementum if the tooth suffers an injury. Note the growth of cementum is relatively slow (by surface apposition) throughout life.
Describe the structure of cementum

What are the different types of cementum?
- The different types of cementum are based on the existence or absence of cementocytes, as well as knowing whether the collagen fibres are extrinsic or intrinsic. Yamamoto et al. (2016) theorised that fibroblasts (and a small number of cementoblasts) produce extrinsic fibres, but only cementoblasts produce intrinsic fibres.
- The extrinsic fibres within acellular extrinsic fibre cementum run perpendicular to the surface of the root and allow the tooth to connect to the alveolar bone by the periodontal ligament (PDL), which is continuous with the cementodentinal junction (CDJ).
- Colard et al. (2016) found acellular cementum only contains extrinsic collagen fibres, whereas cellular cementum contains both extrinsic and intrinsic collagen fibres.
- Nanci (2013) discovered acellular extrinsic fibre cementum to be first cementum to form during tooth development.
- Bosshardt & Selvig (1997) described the acellular layer of cementum as living tissue that typically predominates on the coronal half of the root, whereas cellular cementum occurs more frequently on the apical half.
- Gonçalves et al. (2005) listed the main types of cementum as acellular afibrillar cementum (AAC), acellular extrinsic fibres cementum (AEFC), cellular intrinsic fibres cementum (CIFC) and mixed stratified cementum (MSC).
- Cellular cementum contains cells and is the medium for collagen fibres to attach to the alveolar bone. Ghosh (2019) stated the cellular cementum plays an important role in minor repair of any resorption by continuous deposition in order to maintain the attachment apparatus.
Describe the composition of cementum
- The American Academy of Periodontology (2010) reported that cementum contains about 45 - 50% inorganic material (hydroxylapatite) by weight and about 50 - 55% organic matter and water by weight. Kumar (2011) found the organic component of cementum consists mainly of collagen and proteoglycans.
- Since cementum is avascular (i.e. no blood input), it receives its nutrition through its own imbedded cells from the surrounding vascular periodontal ligament.
- Cementum appears light yellow because it contains the highest fluoride content of all mineralised tissue.
- It is produced continuously throughout life because a new layer of cementum is deposited in order to maintain the attachment as the superficial layer of cementum ages.
- Cementum on the root ends envelops the apical foreman and may stretch onto the inner wall of the pulp canal.
What is the cementoenamel junction (CEJ)?
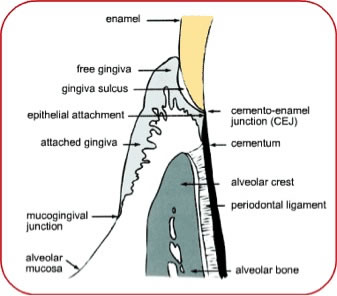
- The cementoenamel junction (CEJ) is the anatomical border between the enamel and the cementum, which is informally known as the neck of the tooth. The CEJ is where the gingiva (gums) connects to a healthy tooth by the gingival fibres.
Describe the formation of CEJ
- In the tooth bud, the enamel organ forms Hertwig's epithelial root sheath, which consists of 2 epithelial layers derived from the external and internal epithelia. The sheath is variably fragmented temporally and spatially as it stimulates cementum deposition on the newly produced dentin.
- After fragmentation, Hertwig's epithelial root sheath becomes involved in cementogenesis and the formation of the periodontal ligament, by forming the epithalial rests of Malassez.
- This variable fragmentation of Hertwig's epithelial root sheath yields an equally variable limit of cervical enamel and a variable onset of formation and deposition of cementum.
- As a result, the relationship between cementum and enamel at the CEJ yields an irregular contour, as observed under a scanning electron microscope.
- Scheid (2012) stated that lack of fragmentation Hertwig's epithelial root sheath will result in enamel deposition that transforms into reduced epithelium, thus prevents cementum deposition on its surface.
Types of CEJ

- Coronal cementum = Where enamel overlaps the cementum
- Abutment (vis a vis relation) = Cementum and enamel converge at the butt joint
- Gap between cementum and enamel, which reveals the dentin
What is the dentinocemental junction?
When the cementoid approaches the required thickness, the cementoid enveloping the cementocytes undergoes mineralisation, which then becomes cementum. When apposition cementum occurs over the dentin, this forms the dentinocemental junction (DCJ). This interface isn't well understood, either clinically or histologically, given that cementum and dentin share common embryological origins.
iv. Pulp
The pulp of the tooth is a collection of connective tissue, blood vessels, nerves, and odontoblasts that constitute the innermost layer of a tooth.
The pulp derives from the dental papilla, in which its cells at the periphery undergo cell division and differentiation to become odontoblasts.
Describe the anatomy of the pulp
- The pulp is the neurovascular bundle inside a tooth that is composed of a central pulp chamber, pulp horns, and radicular canals. The large mass of the pulp is located within the pulp chamber, which resembles the shape of the crown of the tooth.
- Due to the continuous deposition of the dentine, the pulp chamber shrinks with age. Nonetheless, the level of shrinkage throughout the coronal pulp advances quicker on the floor than on the roof or sidewalls.
- Radicular pulp canals continue from the cervical region of the crown to the root apex, which are continuous with the periapical tissues through the apical foramen or foramina.
- Accessory (lateral) canals are pathways from the radicular pulp, which stretch laterally through the dentin to the periodontal tissue. Furthermore, the are located on the lateral surface of the roots of the teeth.
Describe the internal structure of the pulp
The pulp is lined peripherally by a specialised odontogenic area consisting of 4 layers (from innermost to outermost):
-- Pulpal core = Centre of the pulp chamber containing numerous cells and a large vascular supply; except for its location, which is similar to the cell-rich zone.
-- Cell-rich zone = Contains fibroblasts and undifferentiated mesenchymal cells.
-- Cell-free zone = Zone of Weil that contains both capillaries and nerve networks.
-- Odontoblastic layer = Outermost layer that contains odontoblasts and situates next to the predentin and mature dentin.
Cells located in the dental pulp include defence cells like histiocytes, macrophages, granulocytes, mast cells, and plasma cells, as well as fibrobalsts, and odontoblasts. The nerve plexus of Raschkow lies central to the cell-rich zone.
What is the plexus of Raschkow?
- The plexus of Raschkow contains two types of nerve fibres that perceive nociception (pain sensation), which play essential roles in inflammatory events and subsequent tissue repair.
- A-fibres = They are myelinated nerves that conduct fast and sharp pain sensations. A-δ type fibres are preferentially located in the periphery of the pulp, where they are closely associated with the odontoblasts and can extend fibres to numerous but not all dentinal tubules.
- C-fibres = They are unmyelinated nerves that are involved in dull aching pain. The C-Fibres terminate in the pulp tissue proper, either as branches surrounding the blood vessels or as free nerve endings.
- Sensory nerve fibres originating from the inferior and superior alveolar nerves innervate the odontoblastic layer of the pulp cavity. They enter the tooth through apical foramen as myelinated nerve bundles. Then they branch to form the subodontoblastic nerve plexus of Raschkow, which is segregated from the odontoblasts by the cell-free zone of Weil. The plexus of Raschkow is located between the cell-free and cell-rich zones of the pulp.
Nerve supply of the dental pulp
- Schuh et al. (2019) found that a majority of nociceptive sensations occur in the dental pulp due to its high vascularisation and innervation.
- The dental pulp nerve is innervated by cranial nerve 5 (CN V), known as the trigeminal nerve. The nerves enter the pulp cavity through the apical foramen and split off to form the nerve plexus of Raschkow.
- Nerves from the plexus of Raschkow split to form either a marginal plexus around the odontoblasts, or a nerve bundle that penetrates the dentinal tubules.
- Goldberg (2014) stated that the dental pulp is innervated by the sympathetic aspect of the autonomic nervous system. The sympathetic nerves extend into the radicular pulp, where they form a plexus along the blood vessels. In addition, activation of the sympathetic nerves result in vasoconstriction of the blood vessels within the dental pulp, which leads to reduced blood flow in the pulp.
There are main types of sensory nerve fibres in the pulp, each densely located at different sites, which result in different types of sensory stimulation.
What is the function of the pulp?
The functions of the dental pulp include:
- Formation: Production of dentin (by the odontoblasts) that surrounds and protects the pulpal tissue
- Nutrition: Pulp maintains moisture and nutrients levels within the organic parts of the surrounding mineralised tissue.
- Protection / Sensory: Extreme temperature, extreme pressure, or trauma to the dentin or pulp are perceived as pain
- Defence / Repair: Production of reparative or tertiary dentin (by the odontoblasts)
What are the supporting structures?
- One of the tooth's supporting structures is the periodontium, which joins the tooth to surrounding tissues and allows sensations of pressure and touch. It contains the cementum, periodontal ligaments, alveolar bone, and gingiva.
- Cementum is the only supporting structure that is a component of the tooth. The cementum is linked to the alveolar bone by the periodontal ligaments.
- Alveolar bone envelops the roots of teeth in order to provide support and develop an alveolus. The gingiva (gums) is located over the bone, which is visible in the mouth.
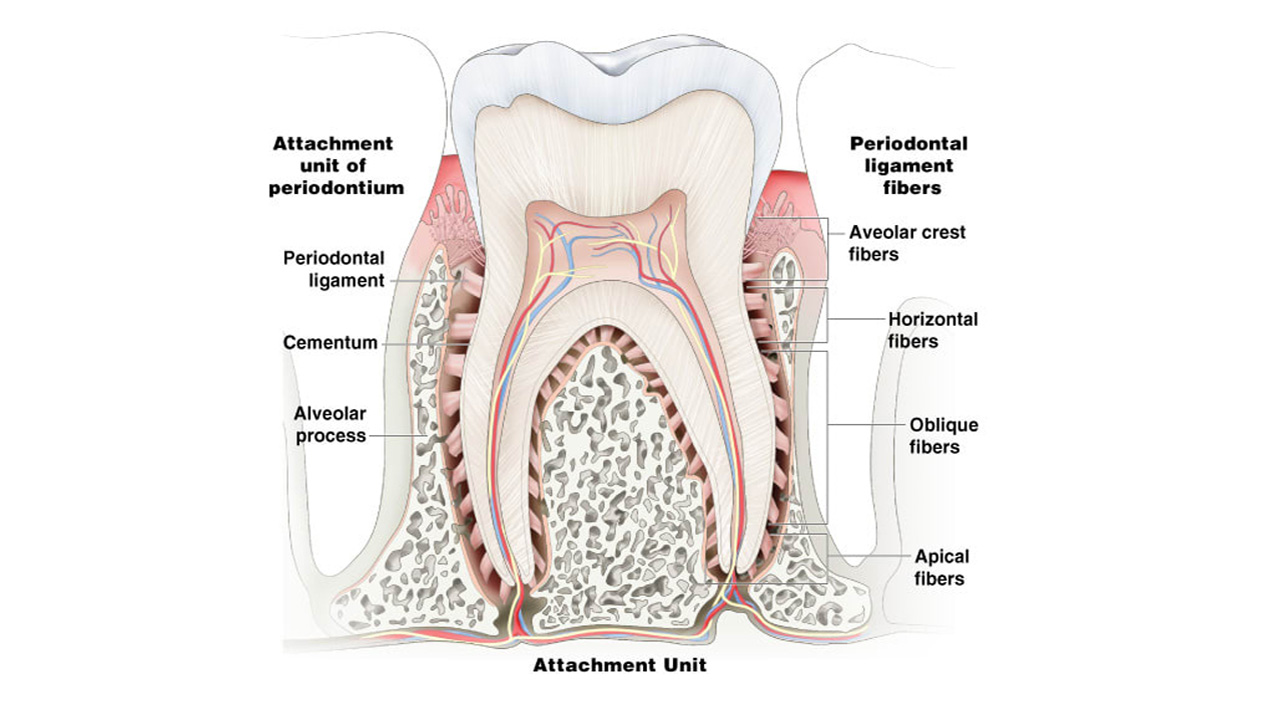
i. Periodontal Ligament
- The periodontal ligament is a specialised connective tissue that joins the tooth's cementum to the alveolar bone. Each ligament is 0.15 - 0.38 mm wide, which reduces in size over time.
- Ross (2002) stated the functions of the periodontal ligaments include support for the tooth, connecting the tooth to the bone, and production and resorption of bone during movement, sensation, and eruption of the tooth.
- Cate (1998) found the periodontal ligament contains a number of cells including cementoblasts, fibroblasts, epithelial cell rests of Malassez, macrophages, osteoblasts and osteoclasts.
- It contains primarily Type I and III collagen, and the ligament fibres are organised in bundles. Listgarten (1999) labelled the bundles of fibres as alveolar crest, horizontal, oblique, periapical, and interradicular fibers.
- Cate (1998) found the nerve supply enters the bone apical to the tooth and creates a neural network around the tooth towards the crest of the gingiva.
- When pressure is applied on a tooth, such as biting or chewing, the tooth shifts in its socket and adds tension on the periodontal ligaments. The nerve fibres then transmits the information to the central nervous system.
ii. Alveolar bone
- The alveobar bone is located on the jaw, forming the alveolus around the teeth. It is produced by osteoblasts and disintegrated by osteoclasts, especially if force is applied to the tooth.
iii. Gingiva
- Known as the "gums", the gingiva is the mucosal tissue that coats the jaws. There are 3 kinds of epithelium associated with the gingiva: junctional epithelium, gingival epithelium, and sulcular epithelium.
- Cate (1998) found these 3 gingiva types derive from a mass of epithelial cells called the epithelial cuff, which is located between the tooth and the mouth.
- Although the gingiva epithelium is visible in the mouth, it doesn't play a direct role in tooth attachment.
- Ross (2002) found the junctional epithelium consists of the basal lamina and hemidesmosomes, which creates an attachment to the tooth.
- Cate (1998) described the sulcular epithelium as non-keratinised stratified squamous tissue on the gingiva that contacts but not attaches to the tooth.
What is tooth eruption?
- Tooth eruption is a process in which new teeth appear through the gums and become visible in the mouth. The mechanism of the tooth eruption process is not well understood and researchers have proposed numerous theories over time that have been disproven. Theories include the Growth Displacement Theory, Continued Bone Formation Theory, and the cushioned hammock theory (proposed by Sicher).
- Edward Harris (2002) suggested the periodontal ligament stimulates tooth eruption by contracting and cross-linking of their collagen fibres, as well as contracting their fibroblasts.
- A new theory based on Wolff's law suggested that the soft tissues surrounding unerupted teeth create sections of tension and compression by distributing the bite forces through the jaws.
- Sarrafpour et al. (2013) suggested these patterns of tension and compression lead to patterns of bone resorption and deposition that elevate the tooth into the mouth. This theory is based on a finite element analysis study that evaluated the distribution of force through the jaw of an 8-year-old child by observing the overall compression in the soft tissues above, and the tension in the soft tissues under, the unerupted teeth.
- Since Wolff's law states that bone resorption occurs when compressed, and forms under tension, this study provides strong evidence for this new theory. However, more research is needed to prove this new theory.
Describe the timeline of tooth eruption
- The tooth buds of baby teeth begin to develop around 6 weeks of pregnancy.
- Adult teeth buds begin to form around 4 months of pregnancy. At this point, the whole tooth begins to form from the crown to the root.
- Primary Dentition Stage: This stage begins around 6 months of age, upon the first appearance of the mandibular central incisors, and ends around 6 years, upon the first appearance of the permanent molars. Humans typically have 20 primary teeth, which erupt in the following order: (1) central incisor, (2) lateral incisor, (3) first molar, (4) canine, and (5) second molar. About 4 primary teeth erupt for every 6 months of life, with eruption of mandibular teeth occurring sooner than the eruption of maxillary teeth, and tooth eruption occurring sooner in females than males.
- Mixed Dentition Stage: This stage begins upon the first appearance of a permanent tooth, which is typically at 5-6 years of age with the 1st permanent molar, and ends until the final primary tooth is lost, typically between 10 and 12 years of age. There are 32 permanent teeth and the maxillary teeth erupt in the following order: (1) first molar (2) central incisor, (3) lateral incisor, (4) first premolar, (5) second premolar, (6) canine, (7) second molar, and (8) third molar. The mandibular teeth erupt in a different order as follows: (1) first molar (2) central incisor, (3) lateral incisor, (4) canine, (5) first premolar, (6) second premolar, (7) second molar, and (8) third molar. A 2005 study discovered no premolars in the primary dentition, and the primary molars were replaced by permanent premolars. A 2005 article by Health Hawaii reported that any primary teeth shed or lost before permanent teeth is in position to replace them, the posterior teeth may deviate forward and result in losing the space in the mouth. This would lead to crowding and/or misplacement upon the eruption of the permanent teeth, known as malocclusion.
- Permanent Dentition Stage: This stage begins when the final primary tooth falls off, typically between 11 and 12 years of age, and lasts for the remainder of the person's life or until all of the teeth have fallen off (edentulism). After the formation of the permanent tooth in the bone, it subsequently pushes through under the primary tooth. Elizabeth Graves (2022) found the adult tooth dissolves the primary tooth's root, which loosens the primary tooth until it falls out. Permanent 3rd molars (wisdom teeth) are often removed due to decay, pain or impaction.
What are the signs and symptoms of tooth eruption?
- The common symptoms of tooth eruption among young eruption is slightly elevated temperature, irritability and drooling, followed by a diarrhoea, fever, rash, reduced appetite, sleeping issues, and vomiting.
- The common signs of tooth eruption include inflammation of the gums and reddening of the gingiva in posterior teeth.
- A 2005 study discovered about 70.5% of children aged between 0 and 36 months of age demonstrated signs and symptoms of tooth eruption such as fever, hyperaemia and/or drooling.
Active vs. Passive Eruption
i. Active Eruption
This refers to the eruption of teeth into the mouth towards the occlusal plane. This is the common path of tooth eruption as all teeth emerge from the gingiva and continue erupting until they contact with the opposing tooth.
ii. Passive Eruption
- Passive eruption describes the apical movement of the gingiva or away from the crown of the tooth to the cementoenamel junction (CEJ) after the complete eruption of the tooth.
- Altered or delayed passive eruption may occur due to problems in the apical migration of the gingival tissue. If the gingival tissues can't move apically, this leads to shorter clinical crowns with more square-shaped teeth, resulting in a gummy smile.
- Coslet et al. (1977) classified delayed passive eruption into 2 types, which associated the bone crest of a tooth to the mucogingival junction (MGJ) of that tooth. These 2 groups are further categorised based on the position of the alveolar bone crest to the cementoenamel junction.
Coslet classification
Coslet et al. (1977) classified delayed passive eruption into 2 types, which associated the bone crest of the tooth to the Mucogingival junction (MGJ) of that tooth. These 2 groups were further categorised according to the position of the alveolar bone crest to the cementoenamel junction.
How are teeth identified?
Nomenclature
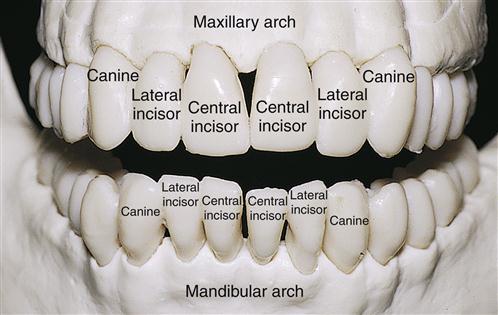
- Teeth are labelled by their sets, as well as their arch, class, type, and side. Teeth are classified into 1 of 2 sets of teeth: primary ("baby", "deciduous') teeth or permanent ("adult") teeth.
- The term "succedaneous" refers to groups of teeth of the permanent dentition that take the place of primary teeth (i.e. canines, incisors, and premolars of the permanent dentition). In addition, the term depends upon which arch the tooth is located in.
- The term "maxillary" refers to teeth in the upper jaw, whereas the term "mandibular" refers to teeth in the lower jaw.
- Deciduous teeth don't contain any premolars, whereas permanent teeth do.
- Incisors are categorised further into central and lateral incisors, premolars are classified further into first and second premolars, and molars are divided further into first, second, and third molars.
What dental notation systems are commonly used?
- The 3 most commonly used systems are the FDI World Dental Federation notation (ISO 3950), the Universal Numbering System, and the Palmer notation.
- The FDI World Dental Federation notation system is used worldwide, whereas the Universal Numbering System is used mainly in the USA.
- In 1947, the committee of the American Dental Association (ADA) recommended the use of the Palmer notation method. However, the Palmer notation method's use of symbols made it difficult to type on keyboards back then. Therefore, the association officially endorsed the the Universal numbering system in 1968.
- Meanwhile, the World Health Organisation and the Fédération Dentaire Internationale officially uses the 2-digit numbering system of the FDI system.
- In 1996, the ADA officially adopted the ISO system as an alternative to the Universal Numbering System.
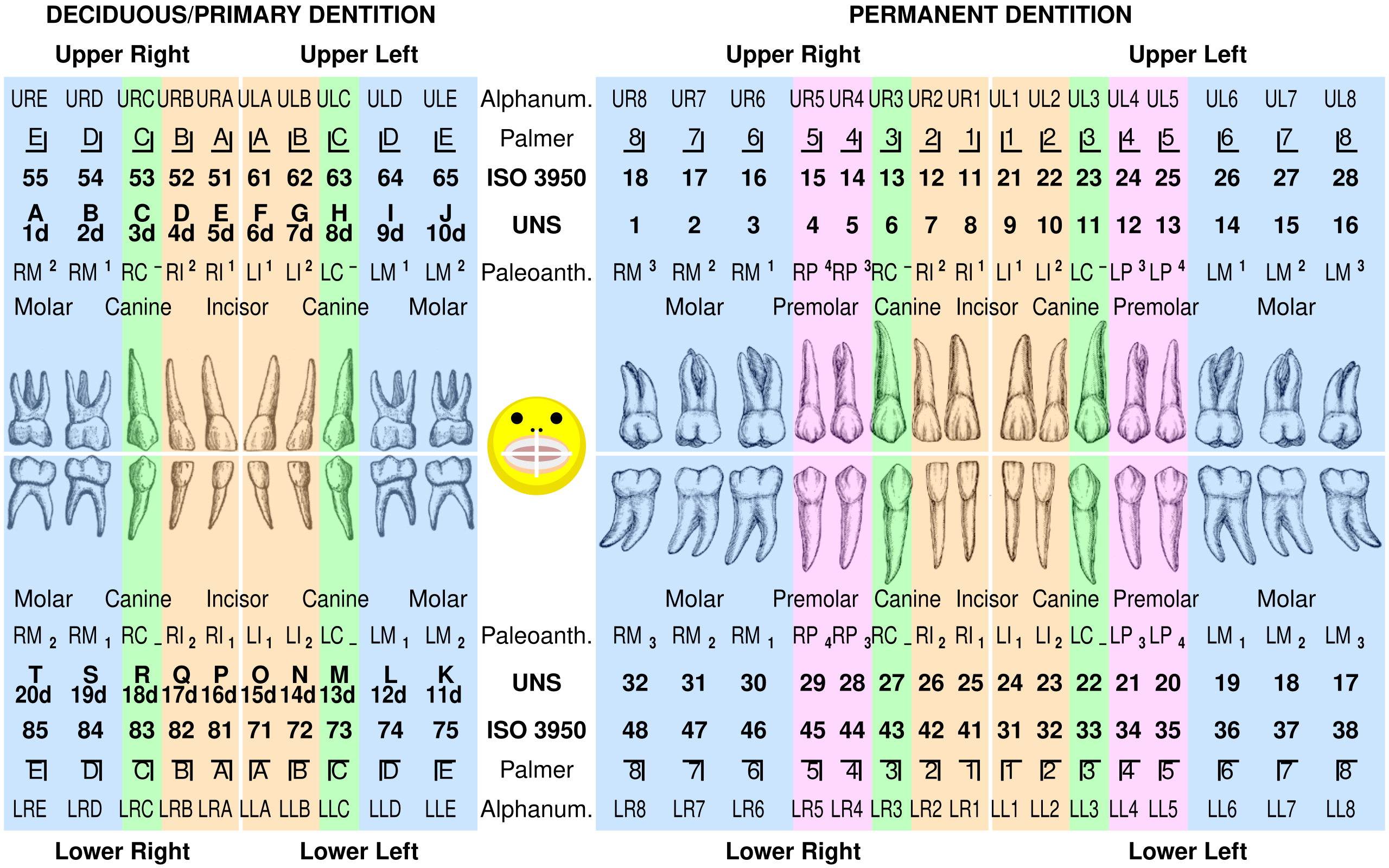
a. FDI World Dental Federation (ISO) notation
- FDI World Dental Federation notation (FDI notation or ISO 3950 notation) is the world's most commonly utilised dental notation. It is denoted by the International Organisation for Standardisation as standard ISO 3950 "Dentistry — Designation system for teeth and areas of the oral cavity".
- This system was developed by the FDI World Dental Federation, which is adopted by the World Health Organisation (WHO), as well as a majority of countries except the USA (which uses the Universal Notation System).
- It allocates 2 numbers to each tooth, one digit to specify the quadrant, and another digit to specify the tooth within that quadrant.
 |
| ISO notation Upper jaw (wisdom teeth removed) |
 |
| ISO notation Lower jaw (wisdom teeth removed) |
b. Palmer notation
![Palmer Notation numbering system [10] | Download Scientific Diagram](https://www.researchgate.net/profile/Ali-Taqi-2/publication/317284562/figure/fig3/AS:500460344037376@1496330453038/Figure-4-Palmer-Notation-numbering-system-10_Q320.jpg)
- Also known as the "Military System", the Palmer notation is named after 19th-century American dentist Dr. Corydon Palmer. Despite the existence of the FDI World Dental Federation notation, this tooth numbering system is preferably used by orthodontists, dental students and practitioners in the UK as of 1998.
- This tooth notation was originally called the Zsigmondy system after Hungarian dentist Adolf Zsigmondy, who first coined the concept of a Zsigmondy cross to record quadrants of tooth positions in 1861. Adult teeth were numbered 1 to 8, and the decidious teeth were described with a quadrant grid using Roman numerals I, II, III, IV and V to number the teeth from the midline.
- Palmer altered the Roman numerals to letters of the alphabet A, B, C, D, and E in order to reduce confusion and the risk of errors in interpretation.
- The Palmer notation contains a symbol (⏌⎿ ⏋⎾) depicting which quadrant the tooth is located and a number denoting its position from the midline.
- Adult teeth are numbered 1 to 8, with deciduous teeth designed by the letters A to E. This would result in the left and right maxillary central incisors indicated by the same number, "1", but the left one would have the symbol "⎿" underneath it, whereas the right one would have "⏌".
c. Universal Numbering System
The Universal Numbering System is a dental notation system primarily used in the USA. The uppercase letters A to T are used for primary teeth and the numbers 1 - 32 are used for permanent teeth. Tooth number 1 is the maxillary right 3rd molar ("wisdom tooth") and the count proceeds along the upper teeth to the left side. After that, the count starts at the mandibular left 3rd molar ("17"), which continues along the bottom teeth to the right side.
Dental charts are typically displayed from the dental practitioner's point of view facing a patient. This means the patient's right side is displayed on the left side of the chart, and vice versa.
 |
| This is a dental practitioner view. Tooth number 1, the rear upper tooth on the patient's right, appears on the left of the chart. |
Describe the anatomy of the tooth
What are the anatomical landmarks of the tooth?
a. Crown and root
- The "anatomic crown" of a tooth refers to the region above the cementoenamel junction (CEJ) or "neck" of the tooth that is coated in enamel. The term "clinical crown" refers to the visible aspects of the tooth in the mouth.
- A greater proportion of the crown consists of dentin, with the pulp chamber situated within. The crown is enclosed within the bone until after the eruption of the tooth, by then it is visible in an anatomically typical and clinically healthy mouth.
- The anatomic root is located beneath the cementoenamel junction and is coated with cementum, whereas the clinical root is any section of the tooth concealed in the mouth.
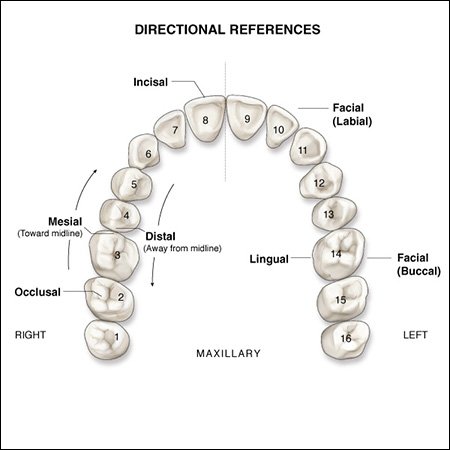
b. Surfaces
- Surfaces closest to the cheeks or lips are denoted as either buccal (situated on posterior teeth adjacent to the cheeks) or labial (situated on anterior teeth adjacent to the lips).
- Surfaces closest to the tongue are referred to as lingual, which may also be denoted as palatal when situated on maxillary teeth next to the hard palate.
- Surfaces that support the chewing process are referred to as occlusal on posterior teeth and incisal on anterior teeth.
- Surfaces adjacent to the junction of the crown and root are denoted as cervical, and those adjacent to the apex of the root are denoted as apical. In addition, the tissue surrounding the apex is referred to as periapical.
- Surfaces adjacent to the median line of the face, which is situated on a vertical axis between the eyes, down the nose, and between the contact of the central incisors, are referred to as mesial. Surfaces located away from the median line are referred to as distal.

c. Cusp
- A cusp is defined as an elevation of the occlusal surface of posterior teeth and canines. Canines typically have 1 cusp, maxillary premolars and mandibular 1st premolars typically have 2 cusps, and mandicular 2nd premolars often have 3 cusps (1 buccal and 2 lingual).
- Maxillary molars usually contain 2 buccal cups and 2 lingual cusps. Sometimes a 5th cusp may form on the maxillary 1st molar called the cusp of Carabelli.
d. Cingulum
- A cingulum is a convexity mesiodistally that looks like a girdle. Henry Gray described the cingulum as an inverted V-shaped ridge.
- It surrounds the lingual surface at the cervical third, and is located on the lingual surface of anterior teeth.
- All anterior teeth are created from 4 centres of development, known as lobes. 3 of those lobes on located on the facial side of the tooth, and one lobe is located on the lingual side.
- Ash & Nelson (2003) found the cingulum forms from the lingual lobe of development. However, a cingulum is typically not well developed or absent on lower incisors. In contrast, a large cingulum is well-developed on maxillary canines.
- A 2007 study by University of Oklahoma College of Dentistry discovered the cingulum of mandibular canines tend to be smoother and rounded.

e. Ridges
Ridges are defined as linear, flat elevations on a tooth, which are named according to their location.
- The buccal ridge runs cervio-occlusally in the centre of the buccal surface of premolars.
- The labial ridge runs cervico-incisally in the centre of the labial surface of canines.
- The lingual ridge runs from the cingulum to the tip of the cusp on the lingual surface of canines.
- The cervical ridge runs mesiodistally on the cervical 3rd of the buccal surface of the crown.
Other ridges include cusp ridges (branching from cusp tips) and marginal ridges (mesial and distal).
- On anterior teeth, they are situated on the mesial and distal borders of the lingual surface. In contrast, on posterior teeth, they are situated on the mesial and distal borders of the occlusal surface.
- Triangular ridges protrude from the cusp tips of premolar and molars to the central groove.
- Transverse ridges are produced by the fusion of 2 triangular ridges on posterior teeth e.g. joining of buccal and lingual triangular ridges.
- The oblique ridge is located on the occlusal surfaces of maxillary molars, which is formed by the fusion of the distal cusp ridge of the mesiolingual cusp and the triangular ridge of the distobuccal cusp. They typically create the distal boundary of the central fossa.
f. Developmental groove
The mandibular central and lateral incisors contain the least amount of developmental grooves. In contrast, canines contain the most prominent developmental grooves, because they anchor to the bone quite strongly.
g. Embrasures
- Embrasures are triangular-shaped spaces situated between the proximal surfaces of neighbouring teeth.
- The interdental papilla of the gingiva, the neighbouring teeth, and the contact point where the two teeth converge form the borders of embrasures.
- There are 4 embrasures for every contact area: cervical (interproximal space), facial (labial or buccal), lingual (palatal), and occlusal (incisal). The cervical embrasure is typically filled by the interdental papilla from the gingiva.
- The main functions of embrasures include the formation of spillways between teeth to guide food away from the gingiva, provision of a self-cleansing mechanism, and gingiva protection from excessive friction trauma as well as modulation of stimulation to the tissues.
h. Mamelons
- Mamelons typically appear as 3 small lumps on the incisal edges of anterior teeth. They are the fragments of 3 lobes of formation of these teeth, with the 4th lobe being associated with the cingulum.
- Mamelons are likely to appear on teeth that have recently erupted into the mouth rather than on older teeth.
Describe the distinguishing characteristics of a tooth
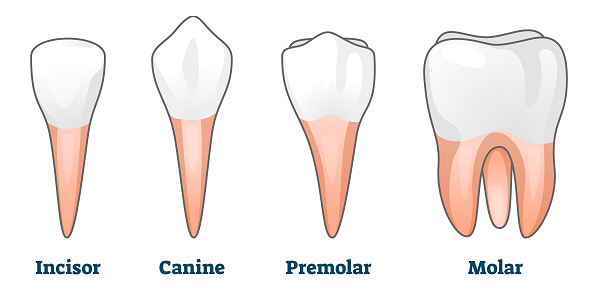

i. Incisors
Incisors are the front teeth existing a majority of mammals. The word incisor comes from the Latin word incidere meaning "to cut". They are found in the premaxilla on the upper jaw and on the mandible on the lower jaw. The main function of incisors in humans is to slice food in to smaller pieces.
Adult humans typically have 8 incisors, 2 of each type. They are:
- Maxillary central incisor (upper jaw, adjacent to the centre of the lips)
- Maxillary lateral incisor (upper jaw, next to the maxillary central incisor)
- Mandibular central incisor (lower jaw, near the centre of the lips)
- Mandibular lateral incisor (lower jaw, next to the mandibular central incisor)
Other animals
a. Maxillary central incisor
- The maxillary central incisor is located in the front upper jaw, and is typically the most visible tooth in the mouth. It is located mesial to the maxillary lateral incisor. It normally has a single cusp on each tooth, known as an incisal ridge / edge.
- The deciduous (baby) set of these teeth form around 14 weeks in utero, and the permanent set forms between 3 and 4 months of age.
- The deciduous maxillary central incisor tooth appears in the mouth between 8 and 12 months of age and fall off between 6 and 7 years of age. The permanent maxillary central incisor tooth replace the deciduous tooth between 7 and 8 years of age.
b. Maxillary lateral incisor
The maxillary lateral incisors are a pair of upper teeth located laterally from both maxillary central incisors of the mouth and medially from the maxillary canines. There are normally no cusps on the teeth, but there is a rare condition called talon cusps are prevalent on the maxillary lateral incisors. The surface area of the tooth involved in eating is referred to as incisal ridge or edge.
c. Mandibular central incisor
- The mandibular central incisor is located on the jaw, adjacent to the midline of the face. It is also located mesially from both mandibular lateral incisors. They are typically the 1st teeth to appear in the mouth, around age of 6 - 8 months.
- There are no cusps on these incisors, but they have an incisal ridge / edge, which is the surface area of the tooth used in eating. Its main functions include cutting or shearing food during mastication.
d. Mandibular lateral incisor
- This tooth is located distally (i.e. away from the midline of the face) from both mandibular central incisors of the mouth and mesially (i.e toward the midline of the face) from both mandibular canines. Their main function is cutting or shearing food during mastication.
- Although there are no cusps, its surface area known as the incisal ridge / edge is involved in the eating process.
ii. Canine (cuspid)
- Also known as cuspids, dogteeth, eye teeth, vampire teeth, or fangs, canine teeth are relatively long, pointed teeth. Canines are developed mainly for the purpose of forcefully holding food in order to tear it to shreds. They tend to be the largest teeth in the mouth of a mammal.
- Mammals typically have 4 canine teeth: 2 in the upper (maxillary) arch and 2 in the lower (mandibular) arch. Canines are situated outside of each lateral incisor and inwards of the premolars.
- Canines are the only teeth that contain a single cusp, and triangular crowns from a mesial view and trapezoidal crowns from a buccal view. Furthermore, the crown of a canine tooth is large and conical, convex on its labial surface, hollow and bumpy on its lingual surface. It reduces to a blunted cusp, which protrudes beyond the level of other teeth.
- The root is singular, conical, compressed laterally, and has a slight groove on each side. The lingual surface contains 2 depressions on either side called the mesial and distal lingual fossae, which are separated by a ridge in between.
- In humans, upper canine teeth eruption usually occurs between 11 and 12 years of age and between 9 and 10 years of age for lower canine teeth eruption.
- Known as baby teeth, the upper deciduous canines usually erupt between 16 and 22 months of age and shed between 10 and 12 years of age. Lower deciduous canines usually erupt between 17 and 22 months of age and shed between 9 and 12 years of age.
- Transposition is a developmental defect commonly observed in the permanant canine tooth, more so with the maxillary than the mandibular. It is described as the positional interchange of 2 adjacent teeth. The upper canine can be transposed with the 1st premolar whilst the lower canine can be transposed with the lateral incisor.
a. Maxillary canine
- The maxillary canine tooth is located laterally from both maxillary lateral incisors of the mouth but mesial from both maxillary first premolars. It is located 3 teeth away from the midline, and separates the premolars from the incisors.
- Maxillary canines start to calcify by around 4 months of age, and the formation of enamel complete by between 6 and 7 years of age. The permanent maxillary canines erupt at between 11 and 12 years of age, and the formation of the root complete by between 13 and 15 years of age.
- The maxillary canines are the longest teeth (from the root to the incisal edge) in the mouth, and are slighter wider than the mandibular canines.
b. Mandibular canine
- The mandibular canine tooth is located distally from both mandibular lateral incisors of the mouth but mesially from both mandibular 1st premolars. It is located 3 teeth away from the midline, and separates the premolars from the incisors.
- The mandibular canines start to calcify at around 4 months of age and the formation of enamel on the crown is complete by around 7 years of age. The permanent mandibular canines start to erupt at between 9 and 10 years of age, with the root of the mandibular canine fully forming by 13 years of age.
iii. Premolar (bicuspid)
- Known as bicuspids, premolars are transitional teeth positioned between the canine and molar teeth. Humans have 2 premolars per quadrant in a permanent set of teeth, meaning they have a total of 8 premolars.
- They are described as 'transitional' for a number of reasons during the mastication process. They contain characteristics of both the canines (lying anteriorly) and molars (lying posteriorly), and food typically transition from the canines to the premolars and finally to the molars where it gets crushed.
- Premolars are referred to as bicuspids (2 main cusps) because they have a buccal cusp and a palatal / lingual cusp which are separated by a mesiodistal occlusal fissure.
The human mouth contains 4 on each jaw, 2 on each side, thus a total of 8 premolars.
Upper jaw (maxillary):
-- Maxillary 1st premolar
-- Maxillary 2nd premolar
Lower jaw (mandibular):
-- Mandibular 1st premolar
-- Mandibular 2nd premolar
a. Maxillary first premolar
- The maxillary 1st premolar is 1 of 2 premolars in the maxilla. They typically erupt at the ages of 10-11, which replace the 1st molars in the primary dentition. It is located behind the canine and ahead of the 2nd premolar.
- The maxillary 1st premolar has 2 cusps, a buccal cusp and a lingual cusp, with the buccal cusp roughly 1 mm taller than the linguak cusp, forming an angular crown. Nelson (2019) described the crown being broader on the buccolingual side compared to the mesiodistal side, which forms a characteristic hexagonal shape when viewed from the occlusal side.
- This tooth normally have 2 roots and 2 root canals, with the buccal root being larger than the lingual root. Olczak et al. (2022) discovered 69% of participants had maxillary 1st molars with 2 roots, 28% had maxillary 1st molars with 1 root, and 3% had maxillary 1st molars with 3 roots.
- Goje & Dave (2024) stated the maxillary 1st premolar erupts between 10 and 11 years of age. Its position is dependent on the position of the erupting maxillary canine.
- The maxillary 1st premolar begins to calcify between 1.5 and 1.75 years of age. The enamel layer is completed formed between 5 and 6 years of age. The oral cavity subsequently erupts between 10 and 11 years of age. Development of the root forms completely between 12 and 13 years of age.
Root Canal System
- The maxillary 1st premolar normally has 2 roots, buccal and palatal, each containing its own root canal, which follow the outline of the respective root.
- The palatal canal is typically bigger than the buccal canal, and the root canals tend to curve towards the buccal side, following the root's outline.
- The cervical 3rd is broader buccolingually, resembling a long, oval, flat or irregular shape, whereas the middle 3rd and apical 3rd are typically oval / long or round respectively.
- The maxillary 1st premolar contains a pulp chamber that considerably wider buccolingually than mesiodistally. Fuller, Denehy & Schulein (2001) found about 70% of maxillary 1st premolars have 2 root canals with separate foramina, and less than 10% contain a single canal and foramen.
- It is estimated about 5% of maxillary 1st premolars contain 3 canals, and the remaining specimens typically have 2 canals that fuse in the apical 3rd, draining through a single foramen.
- The occlusal outline of the pulp chamber consists of 2 pulp horns: the (larger) buccal horn and the (smaller) lingual horn. The concavity of the root is mesial, with the lingual orifice being bigger than the buccal orifice.
- Rajkumar & Ramya (2017) found the presence of 3 canals makes the tooth's external outline more triangular, with the base situated on the buccal side.
b. Maxillary second premolar
The maxillary 2nd premolar is one of two teeth located in the upper jaw, laterally from both the maxillary 1st premolars of the mouth but mesial from both maxillary 1st molars. There are 2 cusps on maxillary 2nd premolars, which are less sharp than those of the maxillary 1st premolars. Although there are no deciduous maxillary premolars, the teeth that preceded the permanent maxillary premolars are the deciduous maxillary molars.
c. Mandibular first premolar
- The mandibular 1st premolar is located laterally from both the mandibular canines of the mouth but mesial from both mandibular 2nd premolars. Mandibular 1st premolars contains 2 cusps: a large and sharp one located on the buccal side of the tooth, and a small and non-functional one located on the lingual side of the tooth. Instead of deciduous (baby) mandibular premolars, there are deciduous mandibular molars.
d. Mandibular second premolar
- The mandibular 2nd premolar is located distally from both mandibular 1st premolars but mesial from both mandibular 1st molars.
- Since there are no deciduous mandibular premolars, the teeth preceding the permanent mandibular premolars are the deciduous mandibular molars.
- This tooth contains 3 cusps: 1 large cusp on the buccal side and 2 smaller cusps on the lingual side. Furthermore, the mesiolingual cusp is twice as large as the distolingual cusp.
iv. Molar
- Molars are large, flat teeth located at the back of the mouth. The term 'molar' derives from the Latin phrase molaris dens, meaning "millstone tooth". The main function of molar teeth is to grind food during the chewing process.
- Adult humans typically have 12 molars, in 4 groups of 3 at the back of the mouth. Each molar contains either 4 or 5 cusps.
- The 3rd, rearmost molar in each group is known as a wisdom tooth, which typically appears later than other molars. It breaks through the front of the gums around the age of 20, although this varies across the human population. In a majority of cases, the wisdom tooth doesn't appear at all.
The human mouth contains 6 on each jaw, 3 on each side, thus a total of 12 molars.
Upper jaw (maxillary):
-- Maxillary 1st molar
-- Maxillary 2nd molar
-- Maxillary 3rd molar
Lower jaw (mandibular):
-- Mandibular 1st molar
-- Mandibular 2nd molar
-- Mandibular 3rd molar
a. Maxillary first molar
The maxillary 1st molar is located laterally (away from the midline of the face) from both maxillary 2nd premolars but mesial (toward the midline of the face) from both maxillary 2nd molars.
The maxillary first molar normally has three root: the mesiobuccal root, the distobuccal root and the palatal root.
- The mesiobuccal root is broad and has pronounced depressions on its mesial and distal surfaces. A majority of mesiobuccal rots have 2 canals, though the internal canal morphology is highly variable.
- The distobuccal root is ovoid in cross section and typically contains one canal.
- The palatal root is more broad mesiodistally than buccolingually and has an ovoidal appearance but typically has one canal. It has a buccal curvature in the apical 3rd, with shallow depressions on the buccal and palatal surfaces.
- J. Craig Baumgartner et al. (2008) measured the average length of the maxillary 1st molar is about 20.5 mm with an average crown length of about 7.5 mm and an average root length of about 13 mm.
b. Maxillary second molar
- The permanent maxillary 2nd molar is located distally from both the maxillary 1st molars of the mouth but mesial from both maxillary 3rd molars.
- In deciduous teeth, the maxillary 2nd molar is the final tooth in the mouth, meaning there is no 3rd maxillary molar behind it.
c. Mandibular first molar
The mandibular 1st molar is located distally from both the mandibular 2nd premolars but mesial from both mandibular 2nd molars. It is situated on the mandibular arch of the mouth, which oppose the maxillary 1st molars and the maxillary 2nd premolar in normal class I occlusion.
- The mandibular 1st molar typically has 5 cusps: the mesiobuccal (MB, toward midline and cheek), mesiolingual (ML, toward midline and tongue), distolingual (DL, away from midline and towards tongue), distobuccal (DB, away from midline and toward cheek), and distal (D, away from midline).
- Viewed from the top (occlusal view), the mandibular 1st molar is pentagonal-shaped and tapers toward the lingual aspect, with the sides being the buccal surface, mesial surface, lingual surface, distal surface, and distobuccal surface.
- The occlusal surface consists of 4 grooves: the central groove, the lingual groove, the buccal groove and the distobuccal groove.
- The central groove runs down the centre of the tooth mesially to distally and contains 4 pits (mesial, central, central, and distal).
- The distobuccal groove runs from the distal pit in the central groove distobuccally bisecting the distal and distobuccal cusps.
- The lingual groove runs from the more distal aspect of the central pits in the central groove toward the lingual surface between the mesiolingual and distolingual cusps.
- The buccal groove runs from the more mesial aspect of the central pits in the central groove toward the buccal surface between the mesiobuccal and distobuccal cusps terminating in the buccal pit.
- The section of the central groove between the central pits is called the Lewis offset, which is an important point to locate the buccal and lingual grooves.
- From the buccal side, there are 2 roots: distal root and mesial root.
- The mesial root is broader buccolingually and has a blunted apex, whereas the distal root is relatively straighter.
- The mesial side show the crown slightly leaning to the lingual side. The mesial root has more prominent flutings than the distal root.
- The height of contour on the buccal side is in the gingival third and the occlusal two thirds of the surface is relatively flat.
- The lingual height of contour is in the middle 3rd of the tooth and the lingual surface is uniformly convex.
d. Mandibular second molar
The mandibular 2nd molar is located distally from both the mandibular 1st molars but mesial from both mandibular 3rd molars. There are typically 4 cusps on the mandibular 2nd molars: 2 on the buccal side and 2 on the lingual side.
e. Maxillary and Mandibular 3rd molar (Wisdom Tooth)
- The mandibular 3rd molar is often referred as the wisdom tooth, which is the most posterior of the 3 molars in each quadrant of human dentition.
- The 3rd molars are described as "wisdom teeth" because they appear relatively later than the other teeth, at an age where people are supposedly "wiser" than as a child, when the other teeth erupt.
- The eruption of wisdom teeth has been known to manifest dental issues for millennia, at least as far back as Aristotle's era. In his 'The History of Animals', Aristotle wrote:
- A 2006 press release at the Field Museum of Natural History reported the oldest known impacted wisdom tooth likely belonged to a European woman who lived between 13,000 and 11,000 BCE, in the Magdalenian period.
Structure of wisdom tooth
- Maxillary 3rd molars have a triangular crown with a deep central fossa from which several irregular fissures arise. Their roots are often fused together to form an irregular shape.
- Mandibular 3rd molars have crowns that have a rounded rectangular shape that consists of 4 or 5 cusps with an irregular fissure pattern. Their roots are significantly shrunk in size and tend to fuse together.
- Rozkovcová, Marková & Dolejsí (1999) found agenesis of wisdom teeth differs by population, ranging from zero in Aboriginal Tasmanians to close to 100% in indigenous Mexicans. Bonczek, Balcar & Šerý (2017) discovered the main factor accounting for this difference is associated with the PAX9 and MSX1 genes, but there is a possibility that other genes may be involved.
- Tsokos (2008) found the reported age of eruption of wisdom teeth varied significantly between different populations. For example, eruption of wisdom teeth occurred earlier in people with African heritage compared to people of Asian and European heritage.
- The most common age range of the eruption of wisdom teeth is between 17 and 21 years of age, but it may begin as early as 13 years of age in some groups. If the wisdom tooth hasn't erupted by the age of 25 years, oral surgeons believe the tooth won't erupt spontaneously.
- Anthropologists theorise human and primate wisdom teeth played a role in mastication of tougher foods. Soft human diets started to become prevalent after the emergence of agriculture and the occurrence of the industrial revolution through the development of tools and cooking to make food easier to chew.
- von Cramon-Taubadel (2011) hypothesised that post-industrial agriculturalist populations encountered less stress chewing food and consequently developed shorter and wider mandibles, compared to hunter-gathered populations. This predisposed them to a number of conditions like dental crowding and malocclusion.
Describe the evolution of the molar in mammals
- In mammals, the crown of the molars and premolars is folded in a variety of complex shapes. The basic components of the crown are the cusps and the valleys in between the cusps. The cusp contains both dentine and enamel, whereas crenulations are produced by differing enamel thickness.
- Cusps sometimes combine to form ridges and expand to form crests. Zhao, Weiss & Stock (200)) described cingula as incomplete ridges that pass around the base of the crown.
- It's theorised mammalian, multicusped cheek teeth evolved from single-cusped teeth in synapsids, but the mechanism of this evolution remains unclear. The "differentiation theory" infers additional cusps have emerged by budding or outgrowth from the crown, whereas the "concrescence theory" suggests that complex teeth evolved by the separate conical teeth clustering together.
- Zhao, Weiss & Stock (2000) concluded therian mammals (e.g. marsupials and placentals) evolved from an ancestor with tribosphenic cheek teeth, which contains 3 main cusps arranged in a triangle.
Comparison of cheek teeth in various taxa: 1, a single-cusped pelycosaur; 2, Dromatherium (a Triassic cynodont); 3, Microconodon (a Triassic eucynodont); 4, Spalacotherium (a Cretaceous "symmetrodont"); 5, Amphitherium (a Jurassic prototribosphenid mammal)
Describe the morphology of molar teeth
- Each major cusp on an upper molar is called a cone and is labelled with a prefix according to its relative location on the tooth: proto-, para-, meta-, hypo-, and ento-.
- The suffixes added to these names include: '-id' for cusps on a lower molar (e.g., protoconid); -ule for a minor cusp (e.g., protoconulid). Myers et al. (2013) described the cingulum as a shelf-like ridge on the left lower section of the crown (on an upper molar). The same feature situated on the lower molar is called a cingulid, and a minor cusp on these is called a cingular cuspule or conulid.
i. Tribosphenic
- Tribosphenic teeth is primarily found in insectivorous mammals such as young platypuses, despite adult platypuses being toothless. In tribosphenic teeth, the lower molar is separated into 2 regions: the 3-cusped trigonid (the shearing end), and the talonid (the crushing heel).
- In modern tribosphenic molars, the trigonid is located towards the front of the jaw and the talonid is located towards the back of the jaw. The trigonid consists of 3 large cusps: the protoconid (on the buccal / labial (cheek) side of the tooth, the anterior paraconid and posterior metaconid (both located on the lingual (tongue) side of the tooth.
- The tribosphenic molars have its protocone cusp on the lingual side of the tooth, whereas the anterior paracone and posterior metacone are both located on the buccal side of the tooth.
- The protocone of the upper molar coordinate with the talonid basin of the lower molar as part of a mechanism to crush food.
- Stokstad (2001) claimed that tribosphenic molars developed independently in monotremes (from australosphenidans), instead of being inherited from a common ancestor shared with marsupials and placentals (from boreosphenidans).
- Luo, Cifelli & Kielan-Jaworowska (2001) found the dentition of the Early Cretaceous monotreme Steropodon resembles that of Peramus and dryolestoids, which indicates a possible link between monotremes and a number of pre-tribosphenic mammals.
- Luo, Ji & Yuan (2007) discovered a number of Jurassic mammalia forms, such as docodonts and shuotheriids, contain a structure similar to talonid grows towards the front of the lower molar, rather than towards the rear. This development is an example of convergent evolution.
ii. Quadrate
- In several groups of species, the hypocone (hypoconid) subsequently emerged from the primitive tribosphenic tooth to form the quadrate (quadritubercular or euthemorphic) molars. The hypocone appears on the lingual (tongue) side of the upper molar, situated posterior to the protocone.
- Quadrate molars are found in numerous species of mammals, including hedgehogs, raccoons, primates, and humans.
- Sometimes, extra smaller cusps appear between the larger cusps of quadrate molars, which are called conules. A paraconule sits between a paracone and a metacone, whereas a hypoconulid sits between a hypoconid and an entoconid.
iii. Bunodont
Bunodont molars contains lower cusps and rounded hills instead of sharp peaks. Bunodont molars are common among omnivores such as bears, humans and pigs. Lawlor (1979) found bunodonts are most effective at crushing material.
iv. Hypsodont
- Flynn, Wyss & Charrier (2007) described hypsodont dentition as high-crowned and an enamel layer stretching past the gum line, which provides additional substance for wear and tear.
- Examples of animals with hypsodont molars include cattle and horses, or any animal that consume gritty, fibrous material. Hypsodont molars continously develops throughout life in some species of Arvicolinea (herbivorous rodents).
- Hypsodont molars don't contain a crown and neck, and its occlusal surface is relatively rough and flat, which indicates it has adapted for crushing and grinding plant material.
- The body of hypsodont molar is covered with cementum above and below the gingival line, with a later of enamel covering the whole length of the body. The cementum and the enamel then invaginate into a thick layer of dentin.
v. Brachydont
- Myers et al. (2013) described brachydont (or brachyodont) as the opposite condition to hypsodont. This kind of dentition is charactirised by low-crowned teeth. For example, human teeth are regarded as brachydont.
- A brachydont tooth contains a crown above the gingival line and a neck below it, as well as at least 1 root. Cementum is only located below the gingival line.
- There is an enamel cap enveloping the crown and stretching down to the neck of the tooth. Paul Kwan (2007) described the occlusal surfaces as pointed, which is suitable for clutching on, tearing and shredding its prey.
vi. Zalambdodont
- Zalambdodont upper molars contain at least 3 main cusps, 1 larger cusp on the lingual side and 2 smaller cusps on the labial side. Crests connect the large cusp with the other 2 cusps to form a narrow V- or λ (lambda)-shape. Myers et al. (2013) found zalambdodont molars are in golden moles, marsupial moles, solendons and tenrecs.
- In zalambdodont placentals, the larger inner cusp is similar to the paracone in a tribosphenic upper molar, whereas the metacone is fused, shrunk or missing. Marsupial moles demonstration the opposite condition, with the paracone missing and the large cusp analogous to the metacone.
- Some golden moles and tenrecs showed their protocone is either missing or shrunk to a smaller 4th cusp, which is located lingual to the large cusp at the tip of the V.
- The 2 labial cusps are found on an expanded shelf called the stylar shelf. In the lower molars, the talonid region is either non-existent or diminished, since it ceased serving as a crushing basin against the protocone.
vii. Dilambdodont
Dilambdodont molars contain a distinct ectoloph, which are shaped like 2 lambdas or a W. The metacone and paracone are on the lingual side (on the bottom of the W), while the stylar shelf is on the labial side. Dilambdodont molars are found in moles, shrews and a number of insectivorous bats.
viii. Lophodont
- Lophodont molar teeth have differentiating patterns of ridges or lophs of enamel integrating the cusps on the crowns. Lawlor (1979) found lophodont teeth are primarily in herbivores, such as mole rats or odd-toed ungulates e.g. equids. Lophodont molars have dense and large enamel ridges called lophs, which are oriented either along or perpendicular to the dental row.
- Myers et al. (2013) found lophodont molars are common in herbivores such as rodents, manatees and tapirs.
- When 2 lophs produce transverse ridges on a tooth, it becomes a bilophodont. Bilophodont molar teeth are common in primates, as well as in rodents and lagomorphs (e.g. hares, rabbits, and pikas).
- The extreme form of lophodonty called loxodonty is found in elephants e.g. (African elephants in the Loxodonta genus) and some rodents (e.g. Otomys).
ix.Selenodont
Named after the mood goddess Selene, selenodont molars contain a major cusp that is elongated into crescent-shaped ridge. They are found in a majority of even-toed ungulates, such as cattle and deer.
x. Secodont (plagiaulacoid)
They are large teeth shaped as a blade used by carnivorous mammals for slicing and chopping. This kind of teeth are also known as carnassials.
iv. Primates
How many teeth does a human usually have?
- Humans typically have 20 primary (or deciduous, "baby", or "milk") teeth and 32 permanent (or adult) teeth). Teeth are categorised as canines, incisors, premolars (bicuspids), and molars. Incisors serve to cut food, canines serve to tear food apart, and molars serve to grind food.
- The 3 most common systems to identify a specific tooth are the FDI World Dental Federation notation (ISO 3950), the Universal Numbering System, and the Palmer notation. The FDI system is used worldwide, whereas the Universal Numbering System is used only in the USA, and the older Palmer notation is used only in the United Kingdom.
v. Rabbits
- Rabbits and other lagomorphs typically shed their deciduous teeth before or shortly after their birth, and are typically born with their permanent teeth.
- Brown (2007) explained that since the rabbit's diet consists of a variety of vegetation that are suffciently abrasive to manifest attribution, their teeth tend to grow continuously throughout their life.
- Rabbits have 6 incisors, 3 upper premolars, 3 upper molars, 2 lower premolars and 2 lower molars on each side, but no canines.
- Ryšavy (2024) discvoered about 3-4 mm of the tooth is eroded every week, whereas the cheek teeth take an extra month to erode the same amount.
vi. Rodents
- Cox & Hautier (2015) found rodents contain upper and lower hypselodont incisors with an enamel layer that grows continuously throughout its life without having properly formed roots. Caceci (2006) described these as aradicular teeth, which rodents must wear down by gnawing on various materials.
- Gomes et al. (2013) found enamel and dentin are produced by the enamel organ, and growth is influenced by the existence of stem cells, cellular amplification, and cellular maturation structures in the odontogenic region.
- The functions of rodent incisors include biting through fruit skin, cutting wood, or for defence. This results in equilibrium rate of wear and tooth growth.
- Thomas Martin (1999) discovered the enamel on rodent incisors are composed of 2 layers: inner portio interna (PI) with Hunter-Schreger bands (HSB) and outer portio externa (PE) with radial enamel (RE).
- Tummers & Thesleff (2003) found the root or crown is associated with the differential regulation of the epithelial stem cell niche in the tooth of 2 rodent species, such as guinea pigs.
- Since rodent teeth have enamel on the outside and exposed dentin on the inside, they self-sharpen as rodents gnaw. Some rodent species, such as the sibling vole and the guinea pig, demonstrate their molars continually grow.
vii. Ungulates
- Cetaceans
- Whale teeth have polyp-like protrusions situated on the root surface of the tooth. These polyps are composed of cementum, with the nodule being located on the inside of the pulp chamber.
- In addition, cementum is located on the entire surface of the whale tooth with a tiny layer of enamel at the tip. A 2011 report stated this tiny enamel layer is only observed in older whales where the cementum has been eroded to reveal the underlying enamel.
- Some species of dolphins bear over 100 teeth in their jaws, whereas narwhals have a giant unicorn-like canine protrusion. The narwhal's canine contains millions of sensory pathways and is used for sensation during feeding, mating, and navigation.
- Beaked whales are virtually toothless, with only a small number of teeth found in males used mainly for feeding.
- Horses
- An adult horse typically as between 36 and 44 teeth, with 12 premolars, 12 molars, and 12 incisors. Furthermore, all male equines have 4 canine teeth between the molars and incisors, whereas a fraction of female horses have about 1-2 canines.
- A few horses are known to have between 1 and 4 wolf teeth, called vestigial premolars, which are likely located in the upper jaw.
- The eruption pattern on milk teeth and then permanent teeth leads to estimates that the horse is under 5 years of age. It is known by the age of 5 years, all permanent horse teeth have erupted.
- The horse's age after 5 years can only be hypothesised by examining the wear patterns on the incisors, the shape, the angle at which the incisors make contact, as well as other factors.
- Once a horse's incisors, premolars, and molars are fully developed, they will continue to erupt as the grinding surface erodes through chewing.
- The length of a young adult horse's teeth is between 110 and 130 mm (between 4.5 and 5 inches), with a large proportion of the crown situated below the gumline in the dental socket. The remaining part of the tooth gradually emerges from the jaw, erupting about 3 mm (1/8 in) each year, as the horse ages.
- When horses approaches old age, the crowns of their teeth are considerably small and they eventually lose such teeth.
- When aged horses lose their molars, they have their food ground up and mixed with water to produce a soft mash for them to eat in order to obtain sufficient nutrition.
Fish teeth
- Many species of fish such as goldfish and loaches have teeth in the pharyngeal arch of the throat.
- Kenneth Karlong (2019) found sharks continually shed their teeth and replace them through a tooth replacement system that effectively replaces their teeth relatively quickly with replacement teeth that are ready to rotate because their teeth often get damaged while catching prey.
- Warmer water temperatures increase the turnover rate of teeth, whereas colder water temperatures decrease the turnover rate of teeth in nurse sharks. Sharks only shed their teeth once new teeth are formed underneath and force them out of the connective tissue that held them in place.
- Purdy & Lonardelli (1995) found female sharks have larger teeth than male sharks because they are, on average, larger in size. In addition, age changes the shape of shark teeth in which baby teeth appearing more narrow and robust, whereas adult teeth are more broad and thin.
- Rücklin et al. (2021) discovered a majority of stem chondrichthyan lineages retained all tooth generations developed throughout the life of the animal. Burrow (2021) found this replacement mechanism is demonstrated by the tooth whorl-based dentitions of acanthodians, such as the Qianodus duplicis, the oldest known tooth vertebrate.
Amphibian teeth
- Pough (2013) found all amphibians contain pedicellate teeth, which consist of connective tissue and uncalcified dentine separating the crown from the base of the tooth.
- Kardong (1995) reported a majority of amphibians have teeth that are attached to the jaw or acrodont teeth, which demonstrate little connection to the dentary and minimal enervation. This helps amphibians use their teeth to grasp their prey but may lose them during feeding if their prey is struggling.
- Xiong (2014) discovered amphibians undergo a metamorphosis to develop bicuspid shaped teeth.
Reptile teeth
- Reptiles such as crocodiles replace its juvenile teeth with larger teeth at a rate as high as 1 new tooth per socket every month. Once the teeth matures, tooth replacement rates begins to reduce to every 2 years and more.
- Poole (1961) estimated crocodiles use around 3,000 teeth throughout their lifetimes.
Bird teeth
- A study by Field et al. (2018) of the Ichthyornis skull suggests the beak of birds may have evolved from teeth in order for chicks to escape their shells after hatching, and therefore evade predators and to perforate protective covers such as hard earth to access underlying food.
Invertebrate teeth

- A 2008 study discovered the parasitic worms of the family Anclostomatidae exhibit such tooth-like structures. For example, the hookworm Necator americanus contains 2 dorsal and 2 ventral cutting plates or teeth around the anterior margin of the buccal capsule. Roberts & Janovy Jr. (2006) discovered a pair of subdorsal teeth and a pair of subventral teeth situated adjacent to the rear.
- Historically used in medicine to remove blood from patients, the European medicinal leech contains 3 jaws that resemble saws in terms of appearance and function. Each jaw contained about 100 sharp teeth used to incise the host. Each incision left a mark sharped like an inverted Y inside of a circle.
- Wells et al. (1993) found that as soon as the medicinal leeches bite, they inject anticoagulants (hirudin) and anaesthetics, then suck out blood, consuming up to 10 times their body weight in a single meal.
- Ruppert, Fox & Barnes (2004) found in some species of Bryozoa, the first section of the stomach forms a muscular gizzard lined with chitinous teeth that can crush armoured prey such as diatoms.
- Similarly, molluscs contain a structure called a radula, which exhibits a line of chitinous teeth. However, these teeth are histologically and developmentally distinct from vertebrate teeth, thus are unlikely to be homologous. Kardong (1995) discovered vertebrate teeth develop from a neural crest mesenchyme-derived dental papilla, and the neural crest being specific to vertebrates.
- Molluscs have a tiny toothed, chitinous ribbon called a radula, which is used for feeding, scraping or cutting food before food enters its oesophagus. Gastropods such as snails and slugs also have a radula for feeding purposes.
- The radula is also used by predatory marine snails such as the Naticidae and the Conidae, as well as predatory pulmonate land slugs such as the ghost slug, and predatory cephalopods such as squid.
- In a majority of ancient lineages of gastropods, the function of the radula is grazing by scraping diatoms and other microscopic algae off rock surfaces and other substrates.
- Asa et al. (2015) found limpets scrape algae from rocks using their radula consisting of hard grinding teeth. It is theorised the tensile strength of the radula is stronger than spider silk.
- Boren (2015) found the mineral protein of the limpet teeth can resist a tensile stress of 4.9 GPa, compared to 4 GPa of spider silk and 0.5 GPa of human teeth.
Fossilisation and taphonomy of teeth
- Archeologists and palaeontologists found early fish such as the thelodonts contained scales constituted of dentine and an enamel-like compound, which indicated that the teeth originated from scales which were retained in the mouth.
- Teaford et al. (2007) discovered fish as early as the late Cambrian contained dentine in their exoskeletons, which was theorised to serve in defence or to sense their environments.
- Lee et al. (2011) found that fossilised teeth are brittle and vulnerable to cracking despite its high resistance. Nevertheless, cracking of the tooth may be useful as a diagnostic tool for estimating the bite force of the animal.
- Fisher (1981) described decalcification as the removal of enamel from teeth with the organic interior layers of dentine and cementin remaining. Decalcification of enamel is accelerated by exposure to plant acids or diagenetic solutions, or in the stomachs of vertebrate predators.
- Fernandez-Jalvo et al. (2002) found enamel can be eroded due to abrasion before dentine or bone gets destroyed by the fossilisation process. In this case, the basic structure of the teeth consists of dentine and a hollow pulp cavity with the organic aspect of dentine disintegrated by alkalis.
How can one maintain oral hygiene?
- Adopting effective oral hygiene habits is essential to keeping your oral cavity clean and free of disease and other issues (such as bad breath). Regular maintenance of oral hygiene plays a critical role in preventing dental disease and bad breath.
- If oral hygiene isn't maintained properly, the most common types of dental disease that manifest are tooth decay (e.g. cavities, dental caries) and gum diseases (e.g. gingivitis, and periodontitis).
What causes most dental issues?
- Known as dental biofilm, dental plaque is a sticky, yellow film containing a diverse range of bacteria that sticks to the surfaces of teeth, which can be easily seen around the gum line. After the tooth surface has been cleaned, it begins to reappear, which is the reason regular teeth brushing is recommended.
- Fejerskov & Kidd (2015) found a high-sugar diet increases the formation of plaque, which increases the risk of tooth decay. This is because the plaque converts sugar into acid, which subsequently weakens the adjacent tooth, resulting in tooth decay.
- If plaque remains on a subgingival surface undisturbed, this not only increases the risk of tooth decay, but also continues to irritate the gums and gives them a redder and swollen appearance.
- If bleeding occurs when you are brushing or flossing your teeth, this indicates a sign of inflammation which suggests poor gum health (gingivitis).
- Another cause of dental problems is dental calculus, which is made of calcium phosphate minerals with live microorganisms that is enveloped by an unmineralised layer. If plaque remains on the tooth surface for an extended period of time, it becomes more firmer and bonded to the tooth. This is known as a calculus and a dental professional has to be consulted to remove it.
- If the calculus is not removed or treated, the ongoing inflammation will result in bone loss and eventually result in the affected teeth becoming loose.
What are the different methods of cleaning teeth?
We are taught to clean our teeth as part of oral hygiene, since it helps remove dental plaque from teeth in order to reduce the risk of cavities, gingivitis, and periodontal disease. The most common methods of teeth cleaning are brushing and flossing, whereas consulting a dental hygienist to clean teeth is less common. Those with dentures and natural teeth typically use a denture cleaner.
i. Brushing teeth
What are the guidelines?
The American Dental Association (2005) provided the following instructions on how to brush teeth.
- Place a small amount of toothpaste on the toothbrush and hold it at a 45-degree angle.
- Gently move the brush in small circular and back and forth motions along the teeth and gums.
- Brush all surfaces inside the mouth, including the tongue. Make sure the back of the teeth (top and bottom rows) are cleaned by brushing vertically in up and down motions.
How frequent should humans brush their teeth?
- A 2008 review by Claydon referenced studies from 1969 to 1973 that concluded teeth brushing more often than every 48 hours helps remove dental plaque, which help maintain gum and tooth health. Furthermore, teeth brushing at intervals longer than 48 hours would result in inflammation of the gums. The review also pointed out that tooth brushing cleans off up to 1 mm of plaque below the gum line, therefore more frequent brushing doesn't clean extra sections of the teeth or mouth.
- Since modern toothpastes have relatively low dentin abrasivity (~ 250), the extra abrasion of dentin from multiple teeth brushings per day seem to be negligible.
- Donly et al. (1997) found 6 months of tooth brushing with manual or sonic toothbrushes didn't significantly wear down the tooth surface or fillings. However, both resulted in a small decrease of cement at the edge of gold inlays.
- Goldstein et al. (2017) conducted a study that simulated 7 years of brushing one side of each tooth with a sonic toothbrush, and subsequently measured the amount of leaking around the fillings. He found no leakage at any bond between the filling and enamel, but found some leakage between filling and cementum on both the brushed and unbrushed sides of the teeth.
- Deinzer et al. (2018) instructed study participants to "brush to the best of their abilities", young adults brushed for longer periods but didn't brush any extra sections of their mouths. The young adults were observed to brush longer on the grinding surfaces of the back teeth, which is where cavities primarily occur in young children, but not in adults. In fact, the sides of the adult human teeth are more susceptible to cavities compared to the grinding surfaces.
- A review by Attin & Hornecker (2005) found consensus that a meticulous tooth brushing once a day is adequate for maintaining oral health, and a majority of dentists recommended patients brush twice a day in the hope that increasing the frequency of brushing would clean additional sections of the mouth.
- Deinzer et al. (2018) concluded that although tooth brushing is the most conventional preventive healthcare activity, the prevalence of tooth and gum disease remains relatively high, since a majority of people clean up to 40% of their tooth margins at the gum line. Furthermore, dental professionals were observed to clean their teeth more effectively compared to laypeople.
Contamination of toothbrushes
- A literature review by Frazelle & Munro (2012) discovered that bacteria survive on toothbrushes for over 24 hours in moist conditions, and less than 24 hours when dried in air, unless they get contaminated by the surrounding environment. If you soak the toothbrushes in mouthwash for about 20 minutes, they can be decontaminated of the harmful bacteria.
- Takenaka, Ohsumi & Noiri (2019) found mouthwashes containing essential oils or chlorhexidine gluconate can eliminate an average of 35% of plaque. However, they didn't mention the extent of simultaneous tooth brushing by the participants in mouthwash studies.
- The side effects of mouthwashes include poor taste and oral irritation (associated with the essential oils and alcohol), as well as calculus, tooth stains, taste disturbance and negative effects on the mouth lining (associated with chlorhexidine gluconate).
What is the optimal technique of tooth brushing?
For conventional toothbrushes:
- Gargle clean, fresh water a few times and rinse the toothbrush with water.
- Brush the front and back of your teeth at a 45-degree angle towards the gum line, moving in a back-and-forth rolling motion in order to make contact with the gum line and tooth.
- To brush the back of your front teeth, hold the toothbrush vertically to the tooth and move in an up-and-down motion.
- To brush the chewing surfaces of the teeth, orient the toothbrush straight at the tooth and brush in a forward-and-back motion.
- If you're using an OralB rotating electric toothbrush, it is recommended to hold the brush against each surface one tooth at a time, follow the shape of each tooth and the gums, and brush for 1-2 seconds per tooth.
- If you're using a Sonicare toothbrush, it is recommended that you hold the toothbrush at a single angle in order for the longer bristles to reach between the teeth, then move in small circular motions 3 - 5 times for 1 - 2 seconds per tooth.
Other techniques include:
- Bass: Focuses on cleaning the regions above and below the gum line with horizontal brush movements.
- Charters: Placing the toothbrush on the gumline at a 45-degree angle toward the biting surface with small rotating motions and short vibrations.
- Fones: A circular motion over the surfaces of the teeth, recommended for children.
- Hirschfeld: A refinement of Fones technique, with the circular motion being smaller and more accentuated over the gum crevice line.
- Modified Bass = Derived from Bass technique, it includes vertical and sweeping motions in order to make circular motions around the gum line.
- Scrub: The toothbrush is placed parallel to the gum line and moves horizontally to "scrub" the gum crevice, chewing surfaces and surfaces adjacent to the tongue.
- Stillman: Similar to the Bass technique, but it involves vertical motions to clean above and below the gum line.
Should you brush your teeth before or after a meal?
- A 2021 article by HuffPost found that brushing immediately after an acidic meal (such as diet soda or common breakfast foods like bread, citrus fruit, coffee, dried fruit, orange juice, or pastries) resulted in additional damage to enamel and dentin compared to a wait time of 30 minutes.
- It is recommended to wash the acid away with water or dissolved baking soda in order to decrease the acid damage manifested by brushing. O'Connor (2012) recommended the same response for acid reflex and consumption of other acidic meals.
- Hannah Seo (2022) concluded that it is prudent to brush before breakfast or dinner rather than brushing immediately after consuming acidic beverages or food.
- Furthermore, brushing your teeth before breakfast helps prevent overnight bacteria accumulation, which in turn helps prevent the bacteria from prospering on high-sugar breakfast foods and reduce the production of acids that damage enamel. In addition, brushing your teeth triggers production of saliva that helps neutralise the acidity and strengthen teeth with essential minerals.
What is a toothbrush?
- A toothbrush is a unique kind of brush aimed at cleaning the teeth, gums, and tongue. It contains a head of compact bundle of bristles, atop of which toothpaste is placed, fixed on a handle where the hand wraps around to facilitate the cleaning of the gums and teeth inside the mouth.
- Humans typically brush their teeth at a sink in the bathroom, where the toothpaste can be spat out and the toothbrush can be rinsed off afterwards to remove any toothpaste foam remaining and then dried to prevent the growth of bacteria or mold.
Describe the history of the toothbrush
- Before the invention of the toothbrush, the chew stick was an early oral hygiene device consisting of twigs with split ends to brush the teeth and a toothpick on the other end.
- Yu, Qian & Zheng (2013) found the earliest chew sticks were discovered in Sumer in southern Mesopotamia dating from 3500 BC, an Egyptian dating from 3000 BC, and in Chinese records dating from 1600 BC.
The Chinese monk Yijing (635 - 713 CE) described in his book the rules for monks when performing the Indian way of using tooth wood for brushing.
"Every day in the morning, a monk must chew a piece of tooth wood to brush his teeth and scrape his tongue, and this must be done in the proper way. Only after one has washed one's hands and mouth may one make salutations. Otherwise both the saluter and the saluted are at fault. In Sanskrit, the tooth wood is known as the dantakastha—danta meaning tooth, and kastha, a piece of wood. It is twelve finger-widths in length. The shortest is not less than eight finger-widths long, resembling
the little finger in size. Chew one end of the wood well for a long while and then brush the teeth with it."
- A number of studies discovered toothpicks were used by the Greeks, Romans and Chinese people during the Qin dynasty, and chew sticks were commonly used by Africans and rural Southern USA.
- In the Islamic world, the miswak is a chewing stick was used as a religious object and is prescribed for use before every prayer, which occurs 5 times a day.
- Sharma et al. (2014) discovered the ancient Indians used the twigs of neem Tree, which are called datun.
 |
| Image of a miswak |
- The first bristle toothbrush resembling the modern toothbrush was discovered in China. Harris (1999) found the early toothbrush used during the Tang dynasty consisted of hog bristles.
- It is theorised the bristles originated from hogs living in Siberia and northern China due to the colder temperatures correlating with rigid bristles. Panati (2013) described the bristles are attached to a handle constructed from bamboo or bone, assembling a toothbrush.
- In 1223, Japanese Zen master Dōgen Kigen recorded in his Shōbōgenzō that he observed monks in China clean their teeth with brushes consisted of horsetail hairs fixed to an ox bone handle.
- Humans that travelled from China to Europe brought the bristle toothbrush with them and it was adopted in Europe during the 17th century. Europeans judged the hog bristle toothbrushes imported from China to be too coarse and preferred softer bristle toothbrushes made of horsehair. Therefore, toothbrushes consisted of horse or boar bristle were mass produced in China and continued to be imported to Britain until the mid-20th century.
- Olmert (1996) found the word 'toothbrush' was first coined in the 1690 autobiography of Anthony Wood who wrote that he had brought a toothbrush from J. Barret.
- According to the Library of Congress (2008), William Addis was thought to be the first person to assemble the first mass-produced toothbrush in 1780 in the UK. In 1770, William Addis was sentenced to Newgate Prison for causing a riot in Spitalfields. During his time in prison, he realised that using a rag with soot and salt was an ineffective method to clean teeth.
- One day, he retrieved a small bone from a meal, drilled small holes into that bone and attached tufts of bristles (that he obtained from one of the guards) into the bone, then inserted the tufts of bristles through the holes in the bone and sealed the holes with glue, creating a toothbrush.
- After his release from prison, he became an entrepreneur and launched a business that manufactured toothbrushes. After his death in 1808, he bequeathed the toothbrush business to his eldest son and it remained within family ownership until 1996.
- The business called Wisdom Toothbrushes was estimated to have manufactured 70 million toothbrushes per year in the UK. By 1840, toothbrushes were being mass-produced in the UK, France, Germany, and Japan. Cheaper toothbrushes contained pig bristles, whereas expensive toothbrushes contained badger hair.
- The Addis Collection is displayed at Hertford Museum, UK, which consists roughly 5000 toothbrushes. The Addis factory located on Ware Road was regarded as a major employer in Hertford until its closure in 1996. Since the closure, Hertford Museum received a bunch of documents and photographs relating to the archive, and collected stories from former employees.
- The first patent for a toothbrush in the USA was granted to H.N.Wadsworth in 1857 (USA Patent #18.653), but mass production of the toothbrush in the USA didn't begin until 1885.
- That toothbrush design consisted of a bone handle with Siberian boar hair bristles placed into the bored holes. However, the issues with animal bristle were the retention of bacteria, inefficient drying after use, and the bristles falling off.
- Mary Bellis (2012) stated that brushing teeth did not become routine in the USA until after WWII, when American soldiers were required to clean their teeth daily.
- Throughout the 20th century, toothbrushes made of bone handles were gradually substituted for toothbrushes made of celluloid. In 1938, DuPont started replacing the natural animal bristles with synthetic fibres, usually nylon.
- The first nylon bristle toothbrush containing nylon yarn was first sold on February 24, 1938. By the turn of the 21st century, nylon bristles had become commonplace and the toothbrush handles were typically created from thermoplastic materials.
- In 1954, the first electric toothbrush was invneted in Switzerland, with the brand name Broxodent.
- In 1978, Dr. George C. Collis created the first toothbrush to contain curved bristles, which follow the curvature of the tooth and safely fit in between the teeth and into the sulcular areas.
In 1977, Johnson & Johnson, introduced the "Reach" toothbrush which differed from conventional toothbrushes in a few ways.
- The Reach toothbrush had an angled head to reach the back of the teeth.
- The bristles are tightly packed in order to clean each tooth of potentially cariogenic materials
- The outer bristles are longer and softer than the inner bristles.
What are different types of toothbrush?
a. Electric Toothbrush
Also known as a motorised toothbrush, or battery-powered toothbrush, an electric toothbrush is a toothbrush that generates rapid bristle oscillations, either in a back-and-forth or rotation (clockwise or counterclockwise) motion, in order to clean teeth.
When was the electric toothbrush invented?
- The first electric toothbrush was produced by Tomlinson Moseley, which was sold as the Motodent, a patent filed by his company, Motodent Inc. on 13th December, 1937.
- In 1954, Dr. Philippe Guy Woog invented the Broxodent, which were originally manufactured in Switzerland for Broxo S.A. He demonstrated the Broxodent can be plugged into a standard wall outlet and operated on line voltage.
- Sean Lee (2009) found the earliest electric toothbrushes were initially produced for patients with limited motor skills and for orthodontic patients (e.g. those with braces).
- In 1960, E.R. Squibb and Sons Pharmaceuticals first produced the Broxo Electric Toothbrush in the USA, which was marketed by Squibb under the names Broxo-Dent or Broxodent. In the 1980s, Squibb transferred the distribution of the Broxodent production line to the Somermet Labs division of Bristol-Myers Squibb.
- In the early 1960s, General Electric (GE) produced an automatic toothbrush that was cordless and power by rechargeable Nickel-Cadmium (NiCad) batteries about the size of a 2-D-cell flashlight handle. This toothbrush came with a charging stand that held the hand piece upright. Since a majority of GE toothbrush units remained in the charger, it wasn't the optimal way to maximise the life of a NiCad battery.
- Early NiCad batteries had a short lifespan and were susceptible to the memory effect. Thus, they were sealed inside the device, and the whole unit needed to be disposed when the batteries eventually failed.
- By the early 1990s, Underwriter Laboratories (UL) and Canadian Standards Association (CSA) no longer certified AC line-voltage appliances for bathroom use because of ongoing problems. Newer electric toothbrushes had to use a step-down transformer for low voltage operation (either 12, 16 or 24 volts).
- Since the 1970s, the wiring standards in numerous countries were updated that forced all outlets in bathroom environments to be fitted with a RCD / GFCI device.
- The first ultrasonic toothbrush, initially named the Ultima and later the Ultrasonex, was patented in the USA in 1992, which was also approved by the FDA for daily home use.
- Initially, the Ultima functioned only on ultrasound, then a few years later, a motor was attached to provide the device additional sonic vibration, which subsequently became the Ultrasonex. Modern ultrasonic toothbrushes simultaneously provide both ultrasound and sonic vibrations.
What are the different types of electric toothbrush?
- Electric toothbrushes are categorised based on the kind of action:
- Side to side vibration = Brush head oscillates laterally from side to side.
- Counter oscillation = Adjacent tufts of bristles (6 - 10) rotate in one direction and then the other direction, independently, with each tuft rotating in the opposite direction to that adjacent to it.
- Rotation oscillation = Brush head rotates in one direction and the other direction.
- Circular = Brush head rotates unidirectionally.
- Ultrasonic = Bristles vibrate at ultrasonic frequencies (> 20 kHz)
- Ionic = The brush relays an electrical charge to the tooth surface that aims to loosen the dental plaque.
- It is recommended that users of a vibrating toothbrush employs a technique similar to a manual toothbrush. In addition, users of toothbrushes with a spinning head are recommended to move the brush slowly from tooth to tooth.
i. Oscillating rotating
- This type of electric toothbrush was first introduced by the Oral-B company in the 1990s. It consists of a small round brush head that oscillates and rotates in order to remove plaque from the tooth surface.
- Grender et al. (2020) found it is similar to the prophylaxis hand piece used by dental professionals to eliminate plaque in the dental office.
- Ralf Adam (2020) discovered the Oral-B iO toothbrush contained a linear magnetic drive system that concentrated energy at the tip of the brush bristles during the oscillating rotating motion. In addition, it uses artificial intelligence to track the toothbrush's position in 3D with an app.
- This allows the user to receive instant feedback on their brushing efficacy, as well as track the data for personalised oral health advice and education from their dental professional.
- The Oral-B iO toothbrush also contains a smart pressure sensor that is electronically calibrated to notify the user if the brushing pressure is too high, or too low. In response, it automatically adjusts the oscillation speed to protect the teeth and gums when excess pressure is applied.
- Van der Weijden et al. (2011) found the oscillating rotating toothbrush is demonstrably safe for both hard and soft tissues of the oral cavity compared to manual toothbrushes.
ii. Sonic
- Sonic toothbrushes are a subset of electric toothbrushes that oscillate rapidly to create vibrations audible to the human ear. A majority of modern rechargeable electric toothbrushes from brands like FOREO, Sonicare, and Oral-B produce frequencies ranging from 200 to 400 Hz, which is equivalent to 12,000 - 24,000 oscillations or 24,000 - 48,000 movements per minute.
- Since sonic toothbrushes solely rely on sweeping motion to clean the teeth, its motion is relatively high in amplitude, which result in significant sweeping movements.
- Tritten & Armitage (1996) found sonic toothbrushes causes less abrasion to the gums compared to the manual toothbrush.
iii. Ultrasonic
- Ultrasonic toothbrushes emit waves at a minimum frequency of 20,000 Hz or 2.4 million movements per minute to clean the teeth. The US Food and Drug Administration (FDA) approved ultrasonic toothbrushes that operate at a frequency of 1.6 MHz, which is about 192 million movements per minute.
- Shinada et al. (1999) found the high frequency and low amplitude vibrations can disrupt bacterial chains in dental plaque, which helps eliminate plaque on the tooth surface up to 5 mm below the gum line.
How effective are electric toothbrushes?
- A 2014 Cochrane review showed that electric toothbrushes remove more plaque and decrease gingival inflammation at a greater rate than manual toothbrushes. For example, using an electric toothbrush for 1 - 3 months reduced plaque build-up by 11% and gingival inflammation by 6%. Furthermore, using a toothbrush for more than 3 months decreased plaque by 21% and decreased gingival inflammation by 11%.
- Awasthi et al. (2015) found electric toothbrushes were beneficial for patients with limited manual dexterity or patients experiencing difficulty reaching the rear teeth.
- Davidovich et al. (2020) deduced that electric toothbrushes are more effective in removing plaque than manual brushes for children.
- Kurtz et al. (2016) discovered the oscillation rotation models of electric toothbrushes removed more plaque than manual toothbrushes. Furthermore, Erbe et al. (2019) found oscillating rotating toothbrushes are more effective in reducing plaque in patients undergoing orthodontic treatment compared to manual toothbrushes.
- Yaacob et al. (2014) concluded only the oscillating rotating electric toothbrush consistently elicited statistically significant benefits over manual toothbrushes.
- Van der Sluijs et al. (2020) inferred that oscillating rotating toothbrushes are more effective than other electric toothbrushes including high frequency sonic power toothbrushes in reducing gingival inflammation and plaque.
- Note that the effectiveness of electric toothbrushes are influenced by factors such as brushing time and the condition of the brush head. Manufacturers recommend changing the brush head every 3 months or as soon as the brush head is noticeably degenerated.
b. Interdental brush
- An interdental or interproximal brush is small, disposable, equipped with an integral handle of a reusable angled plastic handle. Its main use is to clean between the teeth and between the wires of dental braces and the teeth.
- Poklepovic et al. (2013) found a combination of interdental brushes and tooth brushing decreased both the plaque levels and the incidence of gingivitis compared to only tooth brushing. However, more research is required to determine whether it reduces more plaque than dental floss.
- The size of interdental brushes is standardised in ISO 16409. The brush size indicates the passage hole diameter, which is represented by a number between 0 (small space between teeth) and 8 (large space). This correlates with the space between 2 teeth that is sufficiently wide enough for the brush to pass through without bending the wire.
Brush size according to ISO 16409
c. End-tuft brush
- An end-tuft brush contains a small round brush head, which contains 7 tufts of tightly packed soft nylon bristles. The bristles are trimmed so those situated in the centre can reach greater depths into tiny spaces.
- The brush handle is ergonomically designed for a strong grip, providing the control and accuracy required to clean where a majority of other cleaning aids are unable to reach. The areas that are difficult to reach include the tooth surfaces adjacent to missing teeth, crowded teeth, orthodontic structures (i.e. braces), and the posterior of wisdom teeth (3rd molars).
- The end-tuft brush can also clean regions around bridges, dentures, implants and other appliances.
d. Chewable toothbrush
A chewable toothbrush is a small-scale plastic moulded toothbrush that is put inside the mouth. It is considered useful for travellers, which may be available from a number of bathroom vending machines. It is recommended that a chewable toothbrush are disposed after a single use.
e. Musical toothbrush
A musical toothbrush is a manual or battery-powered toothbrush that provides more enjoyment to tooth brushing. It was introduced to children in order to grab their attention and positively impact their tooth brushing behaviour. When the child begins to use the toothbrush, a musical tune starts to play. The toothbrush continuously plays music until the child stops brushing.
What is toothpaste?
- Toothpaste is a gel dentifrice that is usually placed on a toothbrush to clean and maintain the aesthetics and health of teeth.
- It is an abrasive that helps remove dental plaque and food bits from the teeth, suppress halitosis, and provide active ingredients (e.g. fluoride) to prevent tooth decay (dental caries) and gum disease (gingivitis).
When was toothpaste first invented?
- It is thought the Egyptians created a tooth powder since around 5000 BCE, which contains powdered ashes of ox hooves, myrrh, pumice, and powdered and burnt eggshells. Then the Romans improved the tooth powder by adding abrasives such as crushed bones and oyster shells.
- In the 9th century, Iraqi musician and fashion designer Ziryab invented a kind of toothpaste that became popular throughout Islamic Spain. Although the exact ingredients of this toothpaste are unknown, Lebling (2003) reported that it may have been both "functional and pleasant to taste".
- It is unknown whether these early toothpastes were applied alone, were rubbed onto the teeth using rags, or were used with early toothbrushes, such as miswak.
- During the Edo period, Japanese inventor Hiraga Gennai's Hika rakuyo contained advertisements for a "toothpaste in a box" called Sosekiko.
What are the ingredients of toothpaste?
a. Abrasives
- 8 - 20% of toothpaste consists of abrasives, which are insoluble particles that help eliminate plaque from the teeth. Eliminating plaque prevents the accumulation of tartar (calculus), which reduces the risk of gum disease.
- Examples of abrasives include aluminium hydroxide (Al(OH)3), calcium carbonate (CaCO3), hydroxyapatite (Ca5(PO4)3OH), magnesium carbonate (MgCO3), sodium bicarbonate, different kinds of calcium hydrogen phosphates, and different kinds of silicas and zeolites.
- After the Microbead-Free Waters Act of 2015 was passed into US law, the use of microbeads in toothpaste was discontinued in the USA. However, since 2015, the toothpaste industry had transitioned towards FDA-approved "rinse-off" metallised-plasti glitter as their main abrasive agent.
- Some toothpaste contain powdered white mica, which serves as a mild abrasive, as well as gives glittery shimmer to the toothpaste. This toothpaste helps remove stains from the surfaces of teeth by polishing, but there isn't any evidence to demonstrate that it improves dental health compared to the removal of plaque and calculus.
- The abrasive effect of toothpaste is indicated by its RDA value, which shows how severe the erosion of enamel can be when applied to the surfaces of teeth. If the RDA value is above 250, it suggests the toothpaste can be potentially damaging to the surfaces of teeth. Therefore, the American National Standards Institute and American Dental Association characterised toothpastes with an RDA value under 250 to be safe and effective for a lifetime of use.
b. Fluorides
- Fluoride is another common active ingredient in toothpaste as it helps avoid cavities, as well as form dental enamel and bones.
- Common sources of fluoride include sodium fluoride (NaF), stannous fluoride (SnF2), and sodium monofluorophosphate (Na2PO3F).
- At relatively similar fluoride levels, numerous studies found toothpastes containing stannous fluoride were significantly more effective than toothpastes containing sodium fluoride in decreasing the incidence of dental caries and dental erosion.
- Furthermore, a systematic review by Johannsen et al. (2019) concluded toothpastes containing stannous fluoride significantly reduces plaque, gingivitis, staining, calculus and halitosis.
- West et al. (2021) found clinical trials have demonstrated gluconate-chelated stannous fluoride toothpastes provide significantly greater protection against dental erosion and dentine hypersensitivity than toothpastes with or without fluoride.
- A 2019 Cochrane review found American toothpastes containing between 1000 to 1100 parts per million fluoride and European toothpastes containing 0.312% w/w (1,450 ppm fluoride) or stannous fluoride content of 0.454% w/w (1,100 ppm fluoride) correlate with decreased tooth decay.
- Toothpastes with fluoride levels less than 1,000 ppm aren't likely to prevent tooth decay, but the likelihood of this preventive effect increases with concentration.
- Clinical trials revealed that dentifrices with high fluoride levels (5,000 ppm fluoride) significantly decrease the amount of accumulated plaque that help prevent root caries in elderly adults. In addition, it can reduce the levels of mutans streptococci and lactobacilli and stimulate higher calcium fluoride deposits compared to dentifrices containing traditional fluoride.
c. Surfactants
A large number of toothpastes contain surfactants (detergents) such as sodium lauryl sulfate (SLS), which is a foaming agent that allows the consistent dispersal of toothpaste, enhancing its cleansing potential.
d. Other components
-- Antibacterial agents
- A common antibacterial agent in toothpaste is triclosan or zinc chloride, which helps prevent gingivitis and eliminate tartar and bad breath. A meta-analysis by Gunsolley (2006) deduced there was evidence for the effectiveness of triclosan in decreasing plaque and gingivitis.
- Riley & Lamont (2013) discovered that triclosan decreased plaque by 22% and bleeding gums by 48% in gingivitis. However, there was insufficient evidence to suggest toothpastes containing triclosan alleviates periodontitis and has any correlation with the harmful effects of periodontitis for more than 3 years.
- Chlorhexidine is another antimicrobial agent used in toothpastes, though it's more commonly found in mouthwash products. Vranić et al. (2004) found another foaming agent in toothpastes called sodium laureth sulfate, which has antimicrobial effects.
- A systematic meta-review by Janakiram et al. (2020) found that herbal toothpastes containing essential oils, herbal ingredients (such as aloe vera, chamomile, chitosan, neem), and natural or plant extracts (such as hinokitiol) are as effective as non-herbal toothpastes in decreasing dental plaque after 4 weeks of use.
- The stannous (tin) ion in the form of stannous fluoride or stannous chloride has antibacterial effects on the mouth. Cheng et al. (2017) discovered that toothpastes containing stannous fluoride inhibits extracellular polysaccharide (EPS) production in a multi-species biofilm to a greater extent than toothpastes containing sodium fluoride.
- A number of clinical trials have found evidence to deduce that toothpastes containing stannous fluoride significantly decreases plaque and gingivitis compared to other toothpastes.
- West et al. (2021) discovered stabilised stannous fluoride toothpastes protects the teeth against dental erosion and dentine hypersensitivity, which indicates this ingredient serves multiple functions.
-- Flavourants
Companies produce toothpastes in a variety of colours and flavours in order to promote usage of the product. The 3 most common flavourants in toothpaste are peppermint, spearmint, and wintergreen. Flavourants that are uncommon in toothpastes include Anethole anise, apricot, bubblegum, cinnamon, fennel, lavender, neem, ginger, vanilla, lemon, orange, and pine.
-- Remineralising agents
- Known as chemical repair, remineralisation of earth tooth decay is facilitated naturally by the presence of saliva. Various remineralisation agents such as fluoride can enhance this process, but their function is limited by certain factors such as bioavailable calcium.
- Several studies identified casein phosphopeptide stabilised amorphous calcium phosphate (CPP-ACP) as a clinically effective remineralisation agent that augments the action of saliva and fluoride.
-- Miscellaneous components
- Field (2008) discovered a number of agents in toothpaste that prevent it from drying into a powdery form, which include sugar alcohols (e.g. glycerol, sorbitol, or xylitol), and related derivatives (e.g. ,2-propylene glycol and polyethyleneglycol).
- Hu et al. (2018) found arginine and calcium sodium phosphosilicate (CSPS) helps alleviate dentinal hypersensitivity respectively.
e. Xylitol
- Riley et al. (2015) found toothpastes containing xylitol were more effective at preventing dental caries in permanent teeth of children compared to toothpastes containing only fluoride. In addition, xylitol was discovered to not cause any harmful side-effects. Nevertheless, additional research is required to fully understand the efficacy of toothpastes containing xylitol.
ii. Flossing teeth
Dental floss is a cord of thin filaments, usually made of nylon or silk, that is primarily used to remove food and dental plaque from between teeth or sites a toothbrush cannot reach.
When was dental floss invented?
- Dental floss was first invented by an American dentist from New Orleans named Levi Spear Parmly (1790 - 1859). In 1819, he first suggested running a waxen silk thread "through the interstices of the teeth, between their necks and the arches of the gum, to dislodge that irritating matter which no brush can remove and which is the real source of disease."
- However, dental floss wasn't commercially available until 1882, when the Codman and Shurtleft company began producing unwaxed silk floss.
- In 1898, the Johnson & Johnson Corporation received the first patent for dental floss made from the same silk material in silk stiches that doctors use.
- During WW2, physician Charles C. Bass first developed nylon floss, which was more effective than silk floss due to its breater abrasian resistance and potential to be produced in various lengths and sizes.
How often should you floss?
- Dental professionals advise people to floss once per day before or after brushing to reach the areas unreachable by the toothbrush and allow the fluoride from the toothpaste to access areas between the teeth.
- Floss is typically packaged in plastic dispensers that can range between 10 and 100 metres in length.
- This helps take out food particles stuck between teeth and dental plaque that stick to dental surfaces below the gumline.
- Pull out around 40 cm of floss before cutting it with a small blade in the dispenser.
- Hold it between your fingers using both of your hands with about 1–2 cm of floss exposed, or stretch the floss on a fork-like instrument.
- Place the floss between each pair of teeth and gently loop it against the side of the tooth in a 'C' shape and direct it under the gumline.
What are the different types of dental floss?
- There are various types of dental flosses with the most common forms being waxed, unwaxed monofilaments and multi-filaments. Darby & Walsh (2010) demonstrated there is no significant difference between waxed and unwaxed dental floss in terms of effectiveness. However, a number of waxed types of dental floss were found to contain antibacterial agents and/or sodium fluoride.
- Dentists recommend dental tape to people with larger tooth surface area beacuse it is flatter and wider than typical dental floss.
-- Type I = Gums completely fill the embrasure space
-- Type II = Gums partially fill the embrasure space
-- Type III = Gums don't fill the embrasure space.
The table below lists the types of interdental non-powered self-care products available:
The table below lists the different types of Interdental powered self-care products available.
How effective is dental floss?
- A systematic review by Berchier et al. (2008) found flossing was no more effective than tooth brushing along in reducing plaque or gingivitis. Furthermore, they concluded that there is no strong scientific evidence to support regular flossing as an effective therapy for gingivitis patients, and that dental professionals should provide flossing recommendations on an individual basis.
- A systematic review by Sambunjak et al. (2011) discovered strong evidence of flossing combined with tooth brushing decreasing gingivitis compared to solely tooth brushing, but weak evidence of flossing combined with tooth brushing eliminating small amounts of plaque.
- A 2006 review by Chris Longbottom found the risk of tooth decay decreased by 40% in children who flossed their teeth daily over a 1.7 year period.
- A Cochrane Database systematic review by Worthington et al. (2020) compared sole toothbrushing to interdental cleaning devices, as well as compared flossing to other interdental cleaning methods. They concluded that the evidence of flossing being more effective than other interdental cleaning methods is relatively low.
- Imal et al. (2012) found the efficacy of flossing varies depending on personal preference, technique, and determination. Furthermore, flossing may be a relatively more difficult and tedious method of interdental cleaning compared to an interdental brush.
- In 2015, the United States Dietary Guidelines for Americans controversially excluded a recommendation about flossing despite the fact that flossing was recommended as part of an integrated approach to preventing dental diseases in 2000, 2005 and 2010 Dietary Guidelines for Americas published by the U.S. Department of Health and Human Services and the U.S. Department of Agriculture.
- The American Dental Association reached out to the U.S. Department of Health and Human Services about the omission of the flossing recommendation and learnt the reasoning was that the Dietary Guidelines decided to focus on diet rather than skepticism of the efficacy of flossing.
- An HHS spokesperson published an emailed statement that the authors of the 2015 edition decided not to retain the information on brushing and flossing included in past editions of the guidelines because neither the 2010 nor 2015 Advisory Committees reviewed evidence on brushing and flossing teeth.
- However, it's important to understand this doesn't imply flossing is a non-essential oral hygiene practice. In previous editions of the guidelines, flossing was recommended in combination with brushing teeth based on the nutritional recommendation to reduced added sugars.
Floss for orthodontic appliances
- Zanatta & Rosing (2011) found orthodontic appliances, such as bands, brackets, and wires, can retain plaque with more virulent changes in bacterial composition. This would increase gingival recession, cause bleeding on probing, and retain more plaque, which deteriorates periodontal health.
- Srivastava et al. (2013) found fixed appliances restricts the natural cleaning action of the cheek, lips, and tongue to extract food and bacterial debris from tooth surfaces. As a result, this produces new plaque stagnation areas that manifest in the colonisation of pathogenic bacteria.
- Zanatta & Rosing (2011) recommended using dental floss to surface the proximal surface of teeth in combination with toothbrushing in order to maintain plaque control in orthodontic patients.
- Furthermore, a number of clinical studies have shown that correct use of dental floss would result in clinical improvements in proximal gingival health.
Floss threader
A floss threader is a loop of fibre that is used to weave floss into small, unreachable sections around the teeth.
What is a floss pick?
- A floss pick is a disposable oral hygiene device typically composed of plastic and dental floss. It is made up of 2 prongs that extend from a thin plastic body of polystyrene, with a single piece of floss attached to both ends of the prongs. The body of the floss pick narrows at its end to look like a toothpick.
- There are 2 kinds of angled floss picks, the Y-shaped angle and the F-shaped angle floss pick. At the base of the arch, there is a handle to grip and manoeuvre before it narrows off into a pick.
History
- In 1888, B.T. Mason wrapped a fibrous material around a toothpick and named it the "combination tooth pick".
- In 1916, J.P. De L'eau invented a dental floss holder positioned between 2 vertical poles.
- In 1935, F.H. Doner invented the Y-shaped angled dental appliance.
- In 1963, James B. Kirby invented a tooth-cleaning device that resembled an obsolete version of the modern F-shaped floss pick.
- In 1972, Richard L. Wells discovered a technique to attach floss to a single pick end. In the same year, Harry Selig Katz conjured a way to create a disposable dental floss tooth pick.
What is fluoride remineralisation?
- Fluoride catalyses the diffusion of calcium and phosphate into the surface of the tooth, which in turn remineralises the crystalline structures in a dental cavity.
- The fluoridated hydroxyapatite and fluorapatite in the remineralised surfaces protect the tooth from acid attacks, which help avoid dental decay.
- The CDC found a majority of dental professionals and organisations agree that the addition of fluoride in public water has been one of the most successful ways of reducing the prevalence of tooth decay.
- However, a number of groups argued against fluoridated drinking water, citing the neurotoxicity of fluoride or the effects of fluorosis. When a child's teeth is heavily exposed to fluoride, it appears speckled.
- Codes were developed by dental professionals to limit the amount of fluoride intake using filters in water.
- Twetman (2009) found topical fluoride found in toothpaste and mouthwashes don't cause fluorosis, compared to systemic fluoride found in fluorinated water.
What are some common dental procedures?
i. Dental restorations
- A majority of dental restorations involve the removal of enamel in order to access the underlying decaying dentin or inflammation in the pulp.
- Summitt et al. found enamel is first removed from the deep fissures and grooves of a tooth, before a restorative material is added in its place, known as a dental sealant. It is demonstrated dental sealants decrease the risk of future enamal decay by 55% over 7 years.
- Enamel can be removed to add crowns and veneers in order to enhance the aesthetic appearance of the tooth. If the crown or veneer is unsupported by underlying dentin, that section of enamel is more susceptible to fracture.
ii. Acid-etching techniques
- Invented in 1955, acid-etching utilises dental etchants when connecting dental restoration to teeth. Summitt et al. found that by dissolving minerals in enamel, etchants take out the outer 10 μm on the enamel surface and produce a porous layer 5 - 50 μm deep.
- This effectively roughens the enamel and increases the surface area on which the dental restoration can bond.
There are 3 kinds of patterns formed by acid-etching techniques.
- Type 1 = A pattern where the enamel rods are dissolved.
- Type 2 = A pattern where the area around the enamel rods are dissolved.
- Type 3 = A pattern where there is no trace of any enamel rods remaining.
iii. Tooth whitening
- American Dental Hygienists' Association discovered exposure to substances such as coffee, tea, and tobacco can result in discolouration of teeth. The staining occurs in the interprismatic region inside the enamel, which results in the tooth appearing more yellow.
- Chemically, a bleaching agent, such as hydrogen peroxide and carbamide peroxide, is used to initiate an oxidation reaction in the enamel and dentin.
- Oxygen radicals from the peroxide interact with the stains in the interprismatic spaces within the enamel layer. This bleaches the stains, which results in whitening of the teeth. In addition, the whitened teeth reflects more light compared to unbleached teeth, which gives it brighter appearance.
- A 2011 study found whitened teeth doesn't have any ultrastructural or microhardness changes in the dental tissues.
- A tooth whitening product with a relatively low pH can increase the risk of enamel decay by demineralisation, therefore risk evaluation and great care should be taken when considering an acidic product.
- Tooth whiteners in toothpastes contain mild abrasives that help remove stains on enamel, but it doesn't change the intrinsic colour of the tooth. Microabrasion techniques use an acid first to wear out the outer 22 - 27 μm of enamel in order to sufficiently deplete it for the subsequent abrasive force. This results in the removal of superficial stains in the enamel.
Other examples of preventative dental care
Interdental brushes
- Interdental brushes consist of a handle with a piece of wire covered in tapered bristles, which serves to be positioned into the interdental space for plaque removal. Darby & Walsh (2010) found interdental brushes are equally or more effective than floss in terms of plaque removal and reduction of gum inflammation.
Here are the steps in using an interdental brush:
- Identify the size required, the largest size that can fit without force is recommended, if necessary more than 1 size can be used.
- Insert the bristles into the interdental space at a 90-degree angle.
- Move the brush back and forth between the teeth.
- Rinse under water to remove any debris.
- Rinse with warm soapy water once complete and store in a clean dry area.
- Replace once bristles are worn.
Tongue scrapers
- Tongue scrapers are designed to remove any debris accumulated on the tongue that cause halitosis. They can reach the back of the tongue and have strong bristles to remove the debris.
Here are the steps of using a tongue scraper:
- Rinse the tongue scraper first before using it.
- Start scraping at the back of the tongue and gently scrape forwards. Make sure you clean all sides of the tongue, including the middle section.
- Once you have finished cleaning, rinse the tongue scraper to remove any debris stuck on it.
- Rinse the mouth
Oral irrigator
- Also known as a dental water jet, water flosser, or Waterpik, an oral irrigator is a home dental care device that shoots a stream of high-pressure pulsating water into the teeth in order to remove dental plaque and food debris between the teeth and below the gum line. Ng & Lim (2019) stated these devices may promote cleaning for braces and dental implants.
- However, more research is required to confirm oral irrigators can remove plaque biofilm and understand its effectiveness when used by patients with special oral or systemic health needs.
Single-tufted brushes
- Single-tufted toothbrushes are designed to reach locations within the mouth that are difficult to reach. Lee & Moon (2011) suggested this device is optimally used behind the back molars, behind the lower front teeth, on crooked teeth and between spaces where teeth have been removed. Its design consists of an angled handle, a 4mm diameter and rounded bristle tips.
Gum stimulators
- A gum stimulator is designed to massage the gum line and the bases of the regions between the teeth. This aims to increase circulation to the gum line and to eliminate bacteria that might not be cleared away by brushing and flossing alone.
Oral swabs
- Dyck et al. (2012) described oral care swabs (Toothettes) as small sponges attached to a stick, which are often used for oral care in hospitals or long-term care environments. The sponge moistens and eliminates any debris or thickened saliva from the patient's mouth that can't be cleared away by conventional toothbrushing.
What foods and drinks can help with dental care?
- The Academy of General Dentistry recommended eating a balanced diet with low sugar intake can help reduce the risk of tooth decay and periodontal disease.
- The Fédération dentaire internationale (FDI World Dental Federation) and the American Dental Association (ADA) recommended foods such as raw vegetables, cheese, fruit, or plain yogurt as beneficial to dental health.
Chewing gum
Chewing gum helps with oral irrigation between and around the teeth, cleaning and removing debris. However, it is not recommended for unhealthy teeth as it may damage or remove loose fillings. Sugar-free chewing gum can stimulate saliva production, and can aid in cleaning the surface of the teeth.
Other factors that affect dental health
- Dietrich et al. (2007) identified smoking as one of the leading risk factors associated with periodontal diseases. Ryder (2007) found the effects of smoking include impairment of immune responses, inducement of destructive processes as well as inhibition of reparative responses, which increase the risk of periodontal diseases.
- People with an intellectual disability have an elevated risk of developing oral health issues such as dental decay or gum diseases compared to the general population. It is theorised that maintaining oral hygiene isn't one of the main priorities for people with severe disability.
Different types of mouthwash
i. Saline
- Osunde et al. (2014) found the prevalence of alveolar osteitis (dry socket) was reduced in the group that rinsed their mouth with warm saline compared to the control group. Saline is typically recommended after undergoing dental procedures such as dental extractions.
ii. Essential oils (EO) or cetyl pyridinium chloride (CPC)
- Listerine mouthwash contains a bunch of essnetial oils such as eucalyptol, menthol, methyl salicylate and thymol. Other mouthwashes such as Colgate Plax, Crest Pro Health, and Oral B Pro Health Rinse contains cetyl pyridinium chloride (CPC).
- A meta-analysis by Haas et al. (2016) found plaque and gingivitis levels were lower with essential oils mouthrinse when used in addition to a mechanial plaque removal (i.e. toothbrushing and interdental cleaning) compared to cetyl pyridinium chloride (CPC).
iii. Chlorhexidine
- Strydonck et al. (2012) described chlorhexidine gluconate as an antiseptic mouthrinse that should be used in 2-week periods due to brown staining on the teeth and tongue.
- Van Leeuwen et al. (2011) found chlorhexidine is more effective than essential oils in minimising plaque levels, but found no significant positive effect on gingivitis. Therefore, it is primarily used for post-surgical wound healing or the short-term moderation of plaque.
iv. Sodium hypochlorite
- Sodium hypochlorite is a common household bleach that can be used as a 0.2% solution for 30 seconds a few times a week as an affordable and effective means of eliminating harmful bacteria. The commercial product contains about 5-6% sodium hypochlorite, therefore it needs to be diluted by a factor of 30.
Appliances care
i. Dentures
- It is advised that dentures should be cleaned mechanically twice a day with a soft-bristled brush and denture cleansing paste. On the other hand, it is not recommended to use toothpaste because it is too abrasive for acrylic and it will create scratches that retain plaque in the surface.
- Iinuma et al. (2015) recommended the removal dentures at night in order to maintain the protective cleansing and antibacterial properties of saliva against Candida albians (oral thrush) and denture stomatitis, as well as minimise the risk of pneumonia.
- Stafford et al. (1985) recommended that dentures should be stored in a dry container overnight after discovering dry storage of dentures for 8 hours significantly decreases the levels of Candida albicans on an acrylic denture.
- Duyck et al. (2016) recommended soaking a denture overnight approximately once a week with an alkaline-peroxide denture cleansing tablet, which helps decrease bacterial mass and pathogenicity.
ii. Retainers
- It is recommend to clear retainers at least once a day using soap rather than toothpaste and to soak them overnight with an alkaline-peroxide denture cleansing tablet once a week. In addition, it is advised to rinse the retainers under cold water to avoid warping its shape.
- Orthodontics Australia (2020) found storing the retainer in a plastic case and rinsing it beforehand can decrease the amount of bacteria being transferred back into the mouth.
iii. Braces
- For people with braces, it is recommended to use a small or specialised toothbrush with a soft head to access hard-to-reach parts of the teeth. Dr. Akshima Sahi (2020) advised to brush teeth after every meal.
- Benson et al. (2019) found high fluoride toothpaste is more effective than regular toothpaste during treatment. Moreover, applying fluoride foam every 6-8 weeks during treatment could decrease dental decay. However, more research is required to prove this and understand the scientific mechanisms behind it.
- A combination of regular brushing, flossing and floss threaders can help eliminate any accumulated dental plaque, tiny food particles that may get lodged in the braces or between the teeth.
I'll get into the details of appliances used in orthodontics in another post.








































































No comments:
Post a Comment